Wouldn’t it be great if every mom could read her baby’s mind? We feel the same way. Though it may sound impossible, recognizing what your baby is trying to communicate isn’t impossible. Even though babies can’t tell you what they need quite yet, they rely on different sounds and movements to signal when they need to be fed, changed, held, and more long before the crying begins. Though it may not be intuitive right away, with time and close attention, you’ll be able to pick up on your baby’s unique signals and baby’s needs.
After giving birth, one of the most common concerns we hear from new moms is whether their baby is receiving enough milk and being sufficiently fed. Most moms think that crying is the most recognizable hunger cue, but typically, by the time your little one has started crying, they’ve likely been trying to communicate their hunger for some time.
Crying is a late hunger cue—this means that by now, your newborn is probably very hungry, and they are beginning to show distress. Rather than waiting for the waterworks, identifying your little one’s tell-tale signs of hunger and early hunger cues will help improve their health and happiness, along with your own!
If you have been using crying as an indicator of your baby’s hunger, you aren’t alone, and this certainly doesn’t make you a bad mom! Nearly 68% of breastfeeding mothers perceived crying as a cue that their infant wanted to feed. Here’s the good news—there’s an easy fix. Studies show that educating moms on earlier hunger cues makes them much more confident in identifying them in their own children. That’s where we come in! Here are some of the most common baby hunger cues that you should look out for:
Early Infant Hunger Cues
As a new parent, being attentive to early signs of hunger is key to knowing when and how often to feed your child. Beginning to nurse or feed your baby while they’re still calm will facilitate the most successful breastfeeding results. Once crying begins, it can be harder for them to properly latch.
According to the CDC, in the early stages of hunger, newborns tend to:
- Clench their hands into fists
- Bring their hands to their mouth or suck on their hands and fingers
- Pucker, smack, or lick their lips
- Turn their head towards your breast
Other signs may include becoming more alert and active, staring or following you with their eyes, opening and closing their mouth, drooling, sticking out their tongue, and fussing or breathing fast.
It is also important to note that these feeding cues change as your baby ages. While the above signs might indicate hunger in a newborn, new signs may present from around six months to two years after birth. These may include:
- Reaching for or pointing at food
- Opening their mouth when presented with food or a spoon
- Getting excited at the sight of food
- Using their hands or sounds
It kind of goes without saying, but hunger signals definitely get easier to identify and understand as newborns grow into babies, and babies into toddlers.
Is My Baby Eating Enough?
Even after moms can identify hungry baby, many still worry that their baby is not eating enough when they’re being fed to properly satisfy their hunger and nourish their bodies for growth.
Our best advice? Listen to your baby! They will tell you when they are hungry and when they have had enough time at the breast.
Mothers tend to breastfeed their newborns on average eight to 12 times in 24 hours. This frequent nursing schedule helps to regulate your body's breast milk supply to your child's appetite and specific hunger needs. As time progresses and your baby continues to nurse more frequently, they should begin to gain weight.
Typical weight gain for newborns is approximately 4 to 7 oz per week. Most double their birth weight by age 4 to 6 months. Remember: breastfed babies typically put on weight slower than formula-fed infants. This is completely normal and not a cause for concern!
Stomach Size by Age
Being aware of your baby’s stomach capacity will also help to set realistic feeding expectations and create an overall much more enjoyable, worry-free breastfeeding and postpartum experience. Your baby’s belly is much smaller than you probably think it is!
Compared to the average stomach size of an adult (roughly four cups or about the size of a cantaloupe), the stomach capacity of a newborn baby is extremely small. It takes a much smaller amount of milk and nutrients to fill their little stomachs than it does you or even an older child! Anxiety and stress over milk production can actually decrease a woman's breast milk supply substantially, so rather than stressing, remind yourself that your little one has a tiny tummy.
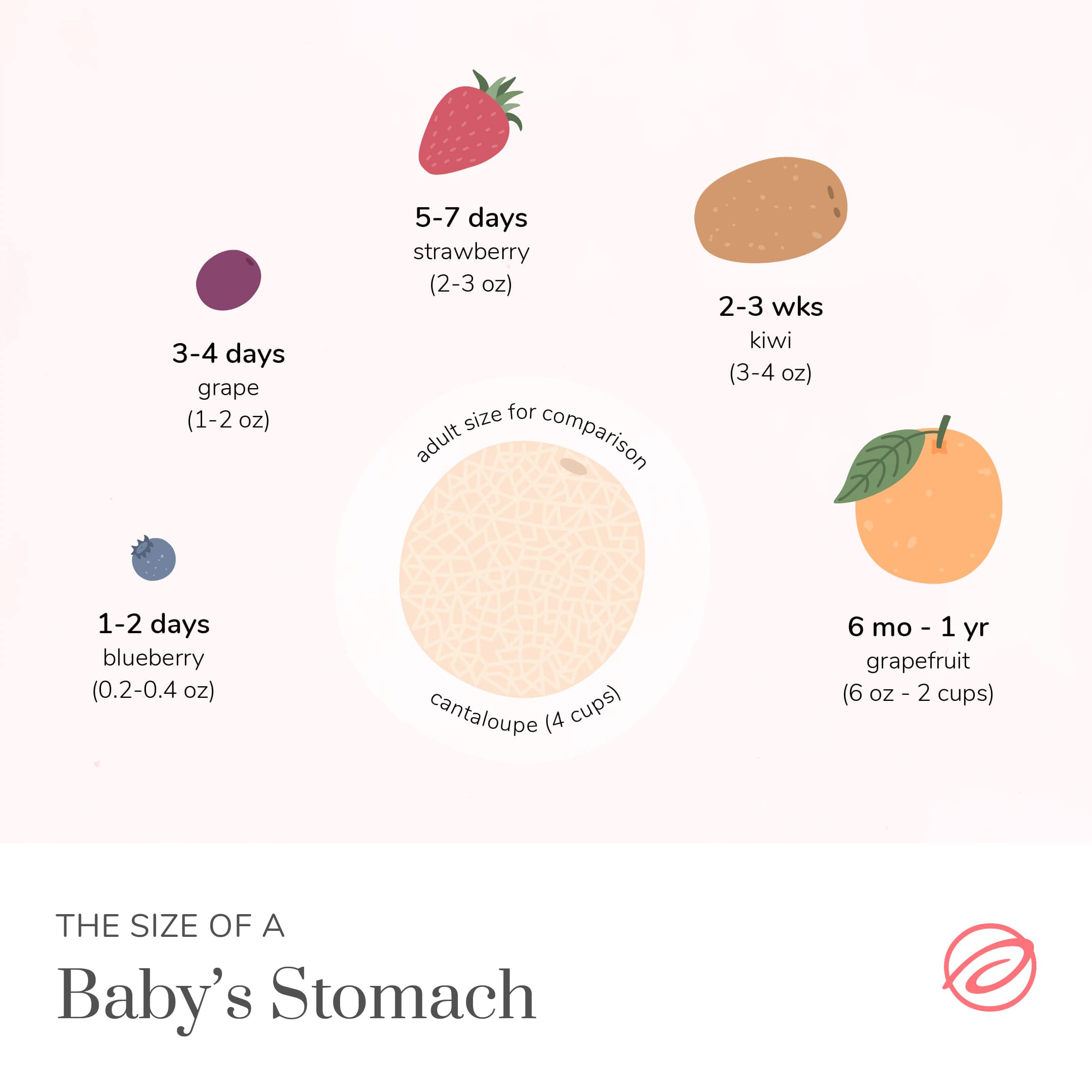
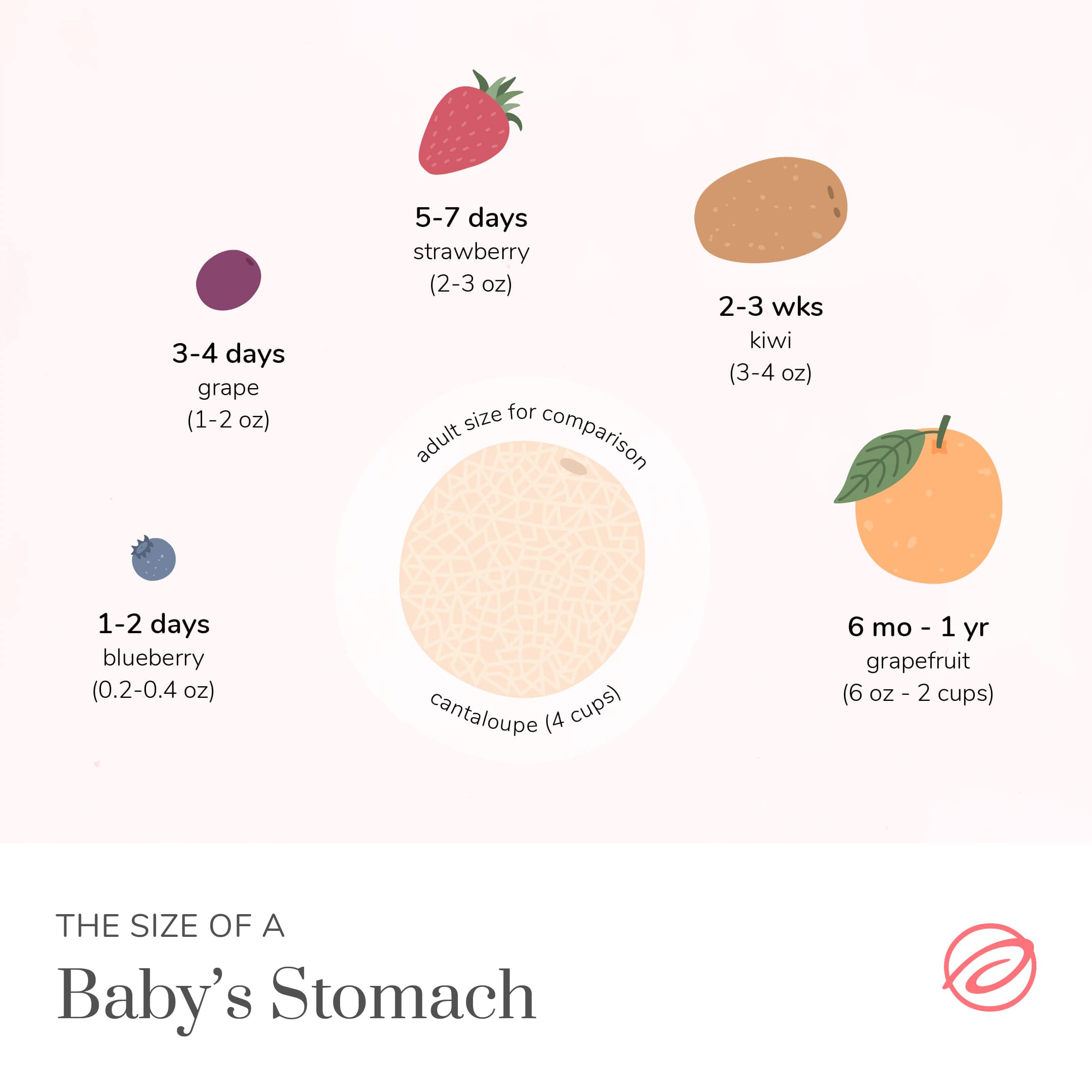
Here is a size breakdown of a newborn stomach by age:
- 1-2 Days: 0.2-0.4 Ounces (about the size of a blueberry)
- 3-4 Days: 1-2 Ounces (about the size of a grape)
- 5-7 Days: 2-3 Ounces (about the size of a strawberry)
- 2-3 Weeks: 3-4 Ounces (about the size of a kiwi)
- 6 Months to 1 Year: 6 Ounces - 2 Cups (about the size of a grapefruit)
Save this chart to help you manage your expectations when breastfeeding, and remind yourself that it doesn’t take much to satisfy your baby’s hunger.
Signs That Your Baby Is Full
It can be difficult to know when your baby has been fed enough, especially because the volume of milk or formula they’re consuming is so small in comparison to the nutritional needs of any other human. The good news is that just like hunger cues, babies also show signs of fullness.
Cues that babies are done eating typically include:
- Closing their mouth
- Turning their head away from your breast
- Opening their clenched hands
- Relaxing their body
Additional signs that your baby is full from feeding include releasing or pushing away from the breast, looking around or showing interest in other things, being content or grinning, or becoming tired and falling asleep.
If your baby seems to be full and is still awake, try burping them, changing their diaper, or switching breastfeeding positions before offering them an additional chance to eat. If your baby is napping, you can skip the burping unless there is a weight concern or other medical condition that requires burping. Check with your healthcare provider to determine if burping is needed after each and every feed.
If, after a diaper change, change of positions, or burping session, your little one doesn’t want to latch, hunger has likely subsided. Feeding patterns will likely change over time, but your child’s cues should remain recognizable. Every child is different and has varying needs and preferences, so learning how to listen to your little one is the best way to ensure they’re getting what they need.
Still Worried They’re Not Eating Enough?
If you’re still worried your baby may not be getting enough milk, talk to a lactation consultant (IBCLC) or your healthcare provider for breastfeeding and medical advice. They can help to improve your overall feeding experience, address if your baby is getting enough milk, answer any questions you may have about what is normal in the first weeks of breastfeeding and pumping, help you overcome specific breastfeeding challenges, and teach you how to properly use a breast pump for optimal milk production. The earlier you reach out with any issues, the better!
When To Start Weaning
According to the AAP and WHO, it is best case scenario for mamas to breastfeed for the first two years. The truth is that everyone is different, and the best time to start weaning is when it is best for you and your baby. If you have specific concerns, consult a physician; otherwise, your child may even let you know that it’s time to wean. Most babies won't self-wean until at least twelve months, but past this, you or your child just may not be interested in breastfeeding anymore—this is a good time to stop.
Looking to pump as part of your breastfeeding journey, and need help getting started? Aeroflow Breastpumps can quickly and easily help you find out if you are eligible to receive a breast pump at little to no cost through your insurance.
Simply complete our Qualify Through Insurance form and let our breast pump specialists take care of the rest! Your dedicated specialist will contact your insurance company and healthcare provider, verify your coverage and network status, and contact you within three to five business days to discuss your pump options and shipment date.
References
https://ideaexchange.uakron.edu/cgi/viewcontent.cgi?article=1057&context=honors_research_projects
https://www.stanfordchildrens.org/en/topic/default?id=slow-or-poor-infant-weight-gain-90-P02880
https://www.cdc.gov/nccdphp/dnpao/growthcharts/who/breastfeeding/index.htm
https://utswmed.org/medblog/decrease-breast-milk-supply/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2720507/











