In 2021, over 30% of babies born in the U.S. were delivered via cesarean section (AKA C-section). While fairly common and generally safe, C-sections are still a major surgical procedure, and the recovery process is very different from that of a vaginal delivery.
Some may elect for a planned C-section. Others may intend on having a vaginal delivery but will end up needing to have an emergency C-section for medical reasons such as placental abruption or high blood pressure. Regardless of your birth plan, all pregnant women deserve to know what to expect from a cesarean delivery and recovery.
The postpartum care and healing process varies from mom to mom, but C-sections tend to be a bit more complicated. Here’s what you need to know about cesarean birth, including our top tips for C-section recovery.
In the Hospital
You’re in the operating room, arms outstretched. Most likely, a blue sheet is placed in front of you, so you can’t see the major surgery occurring on the bottom half of your body. Your pain medication (most likely an epidural/spinal block) should block pain, but you may feel some discomfort and pressure as the physicians perform the C-section.
During a C-section, a surgeon will typically make a transverse incision. This requires two horizontal incisions that are each 4-6 inches long: the first cut—the abdominal incision—is used to open the skin of your lower abdomen (below the belly button near the pubic hairline), and a second incision—the uterine incision—to open the uterus and reach your baby. Rarely, your surgeon may need to make vertical incisions from the belly button to the pubic bone.
Regardless of the mode of delivery, it’s best to hold your new baby skin-to-skin as soon as possible. This can be more challenging after C-section deliveries because your doctors need to maintain a sterile surgical field while they close the incision site. To keep your baby safely on your chest, your providers may place your little one in the “reverse crawl” position, with baby’s head facing down towards your breasts. This will allow your baby to latch and begin breastfeeding without disturbing the surgical field at your abdomen.
The reverse crawl position does require an extra pair of hands for safety and stability, so you’ll need to ask your birth partner or nurse to help you support the baby during feeding. While the reverse crawl isn’t ideal for long-term breastfeeding, it can be an effective way to breastfeed your baby and maintain skin-to-skin contact during the final stages of a C-section delivery.
While you're still in the hospital post-delivery, ask your providers if they used glue, sutures (dissolvable stitches), or staples to close your incision. This will be useful information for future pregnancies if you would like to try for a vaginal birth after cesarean (VBAC).
Regardless of the closure material used, C-section incisions typically take 6-8 weeks to heal, while full physical recovery takes 12+ weeks of healing time.
At Home
Back at home, you may be reflecting back on your birthing experience as you begin the postpartum healing process. It's normal to feel sad if the birth of your little one didn't go the way you envisioned it, but hopefully, when you see your C-section scar, you'll be reminded of your strength, perseverance, and the joy of welcoming your little one into the world.
Your body has natural tools to start the healing process after your C-section delivery, but you can provide some additional care and attention to help your scars heal optimally.
It’s normal for your C-section incision site to be slightly red and tender for the first few weeks postpartum. However, if you notice the redness and tenderness worsening and spreading, particularly in a streaky pattern, call your doctor for a check-up to ensure that you aren’t experiencing surgical complications, like infection at the incision site. Eventually, the scar tissue will flatten out and begin to lighten.
It’s also normal to experience vaginal bleeding after both vaginal birth and C-sections, but you should notify your doctor if you have very heavy bleeding or extreme blood loss that isn’t decreasing over time.
Your health care provider should advise you on basic wound and postoperative care before you leave the hospital, but it’s easy to forget the details in the blur of labor and delivery. Ask your provider to write down any instructions they give you or request help from your birth partner to record these recommendations.
If you know before your due date that you’ll need a C-section, write down any questions you have for your doctor. If you have the opportunity, ask some of these questions during your prenatal appointments.
Incision Care
Your C-section recovery plan should include caring for the incision site to help it heal properly. While your internal uterine incision requires no intervention to heal, your external abdominal incision will. Though your doctor should give you personalized instructions, here are some general guidelines for C-section wound care:
- Employ pain-relieving medication as directed by your health care provider: it’s normal to feel tender and sore at the incision site, especially for the first few days after a C-section delivery. You may experience pain and weakness in your abdominal wall or pelvic pain at the scar site for up to three weeks, but fortunately, it should feel slightly better each day. Your provider may recommend over-the-counter pain medicine like Tylenol™ or Advil™ to help with pain relief to alleviate some of the discomfort.
- It is extremely important that you follow your health care provider’s guidance on pain-relieving medication during this time. When you’re postpartum, you may react differently to medications, even over-the-counter kinds you’ve taken before. Only take medications as instructed by your provider.
- When cleaning the incision site, do not scrub the area, as this can irritate the skin and delay healing. Instead, let warm water gently run over the incision while you’re showering. You can gently clean the area around the incision with soap and water, rinsing thoroughly to remove any leftover soap residue. Gently pat the area dry after showering, and take care to avoid rubbing.
- If your doctor covered your incision with steri-strips, do not remove them. They will fall off on their own after a few days.
- Unless instructed otherwise by your doctor, change any adhesive bandages once a day or more often if they become wet or dirty.
- Do not submerge the wound in water until you receive approval from your doctor. Hold off on baths, hot tubs, and swimming until your provider gives you the all-clear.
- You can place a maxi pad over the incision to absorb drainage from the wound. If you notice drainage or pus that is smelly or greenish-yellow in color, call your health care provider for instructions.
- C-section bandages are a helpful tool for incision care. These waterproof, breathable bandages make it more difficult for bacteria to reach your healing incision. They provide a protective layer that will not slip, rub, or stretch too much, allowing you to participate in your daily activities more comfortably.
While most C-section scars heal well, a cesarean delivery is still major abdominal surgery with all the related risks. Improper wound care during the initial 6-8 weeks after surgery can lead to risk of complications like infection.
Signs of infection include increasing pain, swelling, or redness around the wound; discharge or pus that smells bad; and/or a fever over 100.4 degrees Fahrenheit (38 degrees Celsius). If you are experiencing any of these symptoms, contact your health care provider immediately.
Even if you don't have signs of infection, don’t hesitate to contact your health care provider with questions or concerns.
Your regularly scheduled postpartum appointments are a great time to ask any non-urgent questions about your recovery, including their estimations around your C-section recovery time. Prioritize these appointments, as they are opportunities for your providers to ensure you're on the right track in your postpartum recovery process.
Scar Massage
Have you heard of scar massage? It’s the process of helping your scar heal over time through gentle massage.
In most cases, the surface of your incision will be healed about 6-8 weeks after delivery. Since everyone is different, double-check your own C-section recovery time estimates with your health care provider. Once your provider gives you the all-clear, you can start massaging your scar.
Gentle scar massage may help scar tissue form in the right direction, keeping it from attaching to underlying tissues or becoming keloids or very thick scars (hypertrophic scar formations).
Before beginning scar massage, gather your supplies and wash your hands. Use a lotion or oil to improve glide and reduce friction on your skin: aloe vera gel or vitamin E oil are great, safe options!
Pro Tip: Give yourself a scar massage right after a warm shower. Your hands will already be clean, and the heat from the shower makes your skin more pliable.
You may notice the area around your C-section incision feels numb but also sensitive. As counterintuitive as that may sound, this is common! Massaging the area regularly may help normalize your sensation in the area. Remember: It can take many months to regain sensation, so don’t panic if you don’t notice immediate changes.
To begin:
- Apply your lotion or oil of choice to the scar site and the skin surrounding it.
- Use the pads of 2-3 fingers to gently press on the skin surrounding the incision site, moving your hand in a circular motion. No need to press down hard: massaging too aggressively can be counterproductive for wound healing. Scar massage should not be painful!
- Continue these circular motions on the skin above, below, and beside the scar itself.
- After a minute or so, switch to massaging the area using vertical (up and down) and horizontal (side-to-side) movements.
- When you feel ready, you can begin massaging over the scar directly. It’s normal for the scar itself to feel numb or slightly tender, but again, this should not hurt!
- Spend 5–10 minutes per day massaging on and around the scar.
Additional Recovery Tips
The First Two Weeks: Prioritize Rest
Rest should be your top priority during C-section recovery. It may feel harder to rest after you’ve left the hospital or birthing center (especially if you have other kids at home), but it’s critical to take it easy for at least the first two weeks after your C-section. Now is not the time to push yourself!
Here are some tips to make rest a reality:
- Take advantage of offers from your family members and friends. Let them help you by cleaning your house, running your errands, and preparing your food.
- Avoid lifting anything heavier than your baby for the first 2-4 weeks postpartum.
- Limit pushing and pulling motions (like pushing and pulling a vacuum cleaner) as much as possible.
- Sleep as much as you can! You may not always be able to sleep when the baby is sleeping, but take every opportunity you get to grab a nap.
Get Moving
After rest, gentle motion is the second most important thing you can do to help your body heal in the early weeks after a C-section.
In the first few hours after surgery, your hospital care team will monitor you closely as the anesthetic (numbing agent) wears off. During this time, your health care team will remove your urinary catheter and encourage you to drink plenty of water.
There’s nothing like a full bladder to encourage you to get up and move around! Your care team will instruct you on how to begin gentle movement, and they’ll help you get out of your hospital bed to start walking. Gentle movement like walking improves blood flow, which helps prevent blood clots and other common surgical complications. Here are some tips for making movement easier in those first few hours after giving birth.
- Avoid sitting straight up in bed, as this strains your recovering abdominal muscles. Instead, roll to one side and let your legs dangle off the side of the bed. Use your arms to push yourself up into a sitting position.
- Use your breathing to help you manage movement and pain. Exhale as you transition from lying to sitting and from sitting to standing. Breathing out reduces pressure on your incision site and helps to calm sensitive nerves.
- To support your healing belly, you can gently press a pillow over your lower abdomen. This external support can reduce discomfort during transitions in the early days post-op.
Your recovery continues even after you’ve left the hospital or birthing center. Here are some tips for incorporating regular movement into your C-section recovery plan:
- After you've returned home, continue walking around your house throughout the day. If possible, avoid stairs for the first several weeks. If you must climb the stairs, hold on to the railing and take it very slowly.
- Movement will gradually get easier, but it’s normal to feel achy and sore for the first few days of postpartum. This discomfort should improve a little bit each day as you heal and become more mobile. If you suddenly feel worse, call your OB-GYN as soon as possible and ask for a check-up.
- If you experience any chest pain or shortness of breath, please contact your primary care doctor immediately, as this could be a sign of a pulmonary embolism.
Stay Hydrated
The medications you were given during surgery can slow down your digestive system and may lead to constipation. You can combat postpartum constipation in several ways:
- Stay hydrated by drinking at least three quarts of water each day. (start this hydration habit before delivery for the best effect!)
- Eat fiber-rich foods like whole grains, juicy fruits, and crunchy veggies to improve the consistency of your stool.
- Ask your health care provider if you can use a stool softener or fiber supplement to assist with bowel movements. Remember, your postpartum body may react differently to medication than it did before pregnancy. Always ask your doctor before starting a new medication, even an over-the-counter type.
A bonus if you plan to breastfeed: staying hydrated supports your breast milk supply, too!
Practice Breathwork
We’ve already touched on the value of breathing to help you manage pain and movement in the early days after surgery. Reconnecting with your breath is a great first step to reconnect with your postpartum body!
Simple breathing techniques can help calm your mind, restore the connection between mind and body, and even kickstart the healing of your abdominal muscles. Here’s how to get started:
- Inhale through your nose, allowing your lungs to fill until you feel your ribs expanding toward the front and the back of your body.
- Allow your abdomen to fill as you breathe in. It helps to rest a hand on your lower ribs and upper belly so you can feel your body expand.
- Exhale completely through your nose or mouth. Allow your belly and ribs to empty like a balloon deflating.
- Repeat this pattern of slow, deep breaths for several minutes.
Postpartum Recovery Garments
Regardless of your mode of delivery, your back, pelvic floor, and abdomen do a lot of hard work during pregnancy and delivery, and they may need a little extra support. Because C-section incisions cut through your abdominal muscles, using a support garment during your C-section recovery can be a game changer.
Postpartum recovery garments are designed to support your abdomen and incision site from the outside. This extra support can help alleviate some pain you may feel when you cough, sneeze, or even laugh.
As you return to everyday activities, a postpartum recovery garment provides gentle compression to reduce swelling, stabilize your abdomen, and support your lower back and hips.
Recovery garments aren’t designed for indefinite use—think of them as a tool to assist the rehabilitation of your muscles. A pelvic physical therapist or postpartum corrective exercise specialist can guide you through a comprehensive core recovery plan.
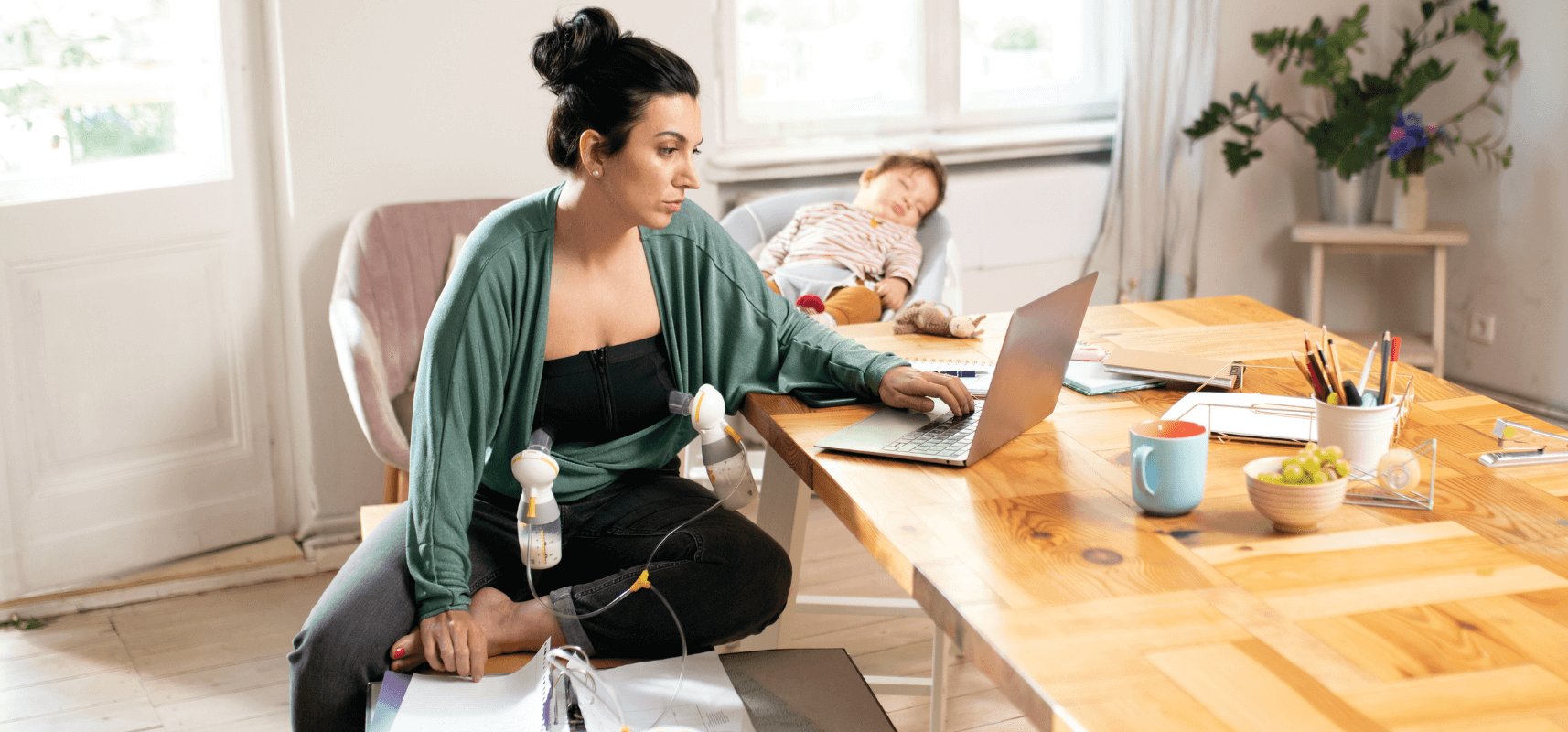
Breastfeeding Positions
Everyone's breastfeeding experience is different. There is no one-size-fits-all guide, especially after a C-section delivery. You may find that it’s difficult to find a breastfeeding position that doesn’t put pressure on your incision, or maybe the breastfeeding position you used during a previous vaginal delivery is no longer comfortable. If you're struggling to find a position that works, a lactation consultant can help you troubleshoot and answer any questions you may have.
Here are 6 lactation-consultant-approved breastfeeding positions that are great for mamas who’ve recently had a cesarean section:
Football Hold
In this upright position, sit upright with your back supported by a chair. Hold your baby off to one side so they are less likely to kick or rub against your incision. This is best to use early on before your baby becomes too large to manage in this position.


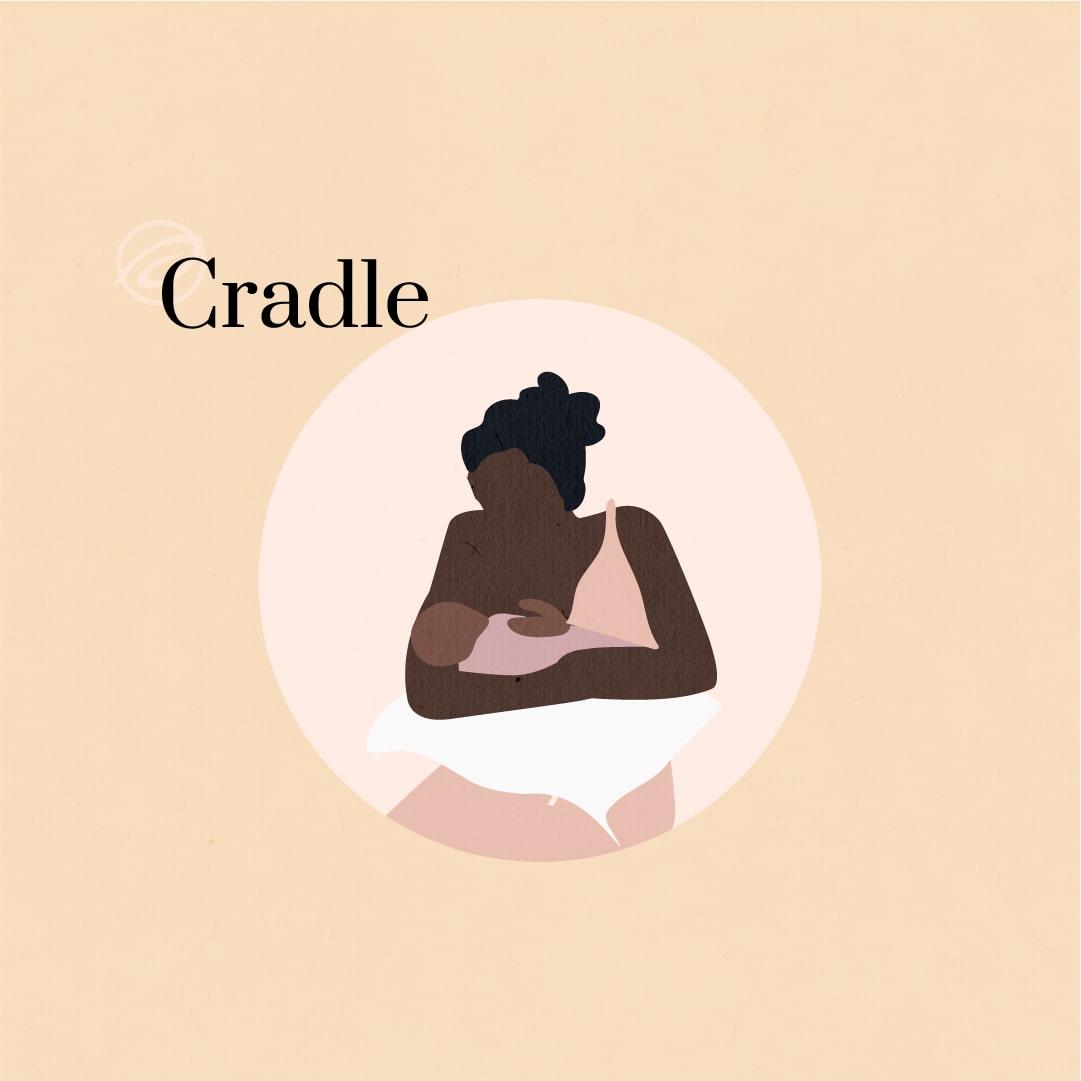
Cradle Hold
For this classic breastfeeding position, sit upright with your back supported and your baby positioned on their side. Rest the baby’s head and neck along your left* forearm so they can latch to your left breast. Your baby’s body will rest against your upper stomach, above the level of your incision.
*This position will usually feel natural to right-handed breastfeeders. If you’re a lefty, you may feel better switching sides so your baby latches to your right breast.
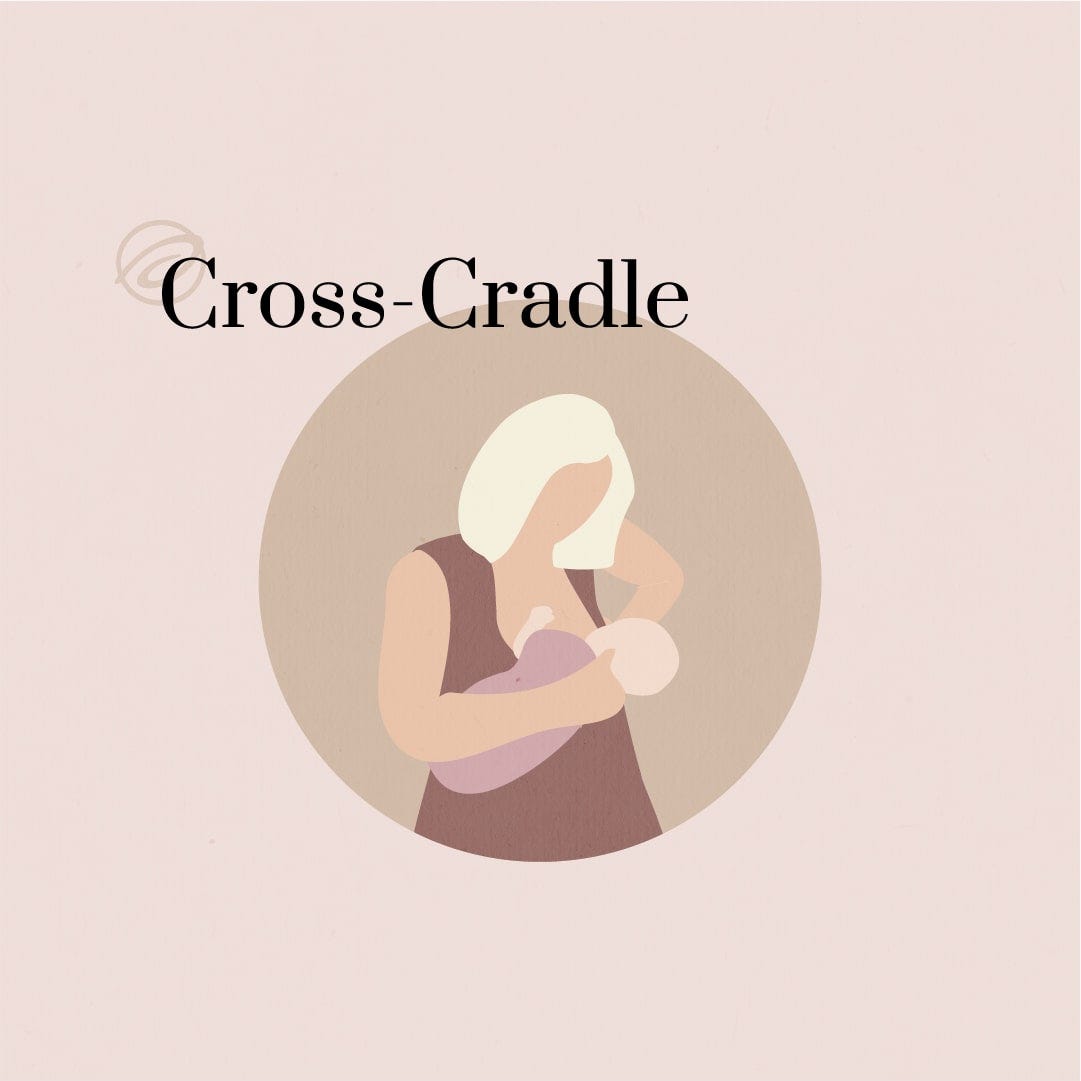
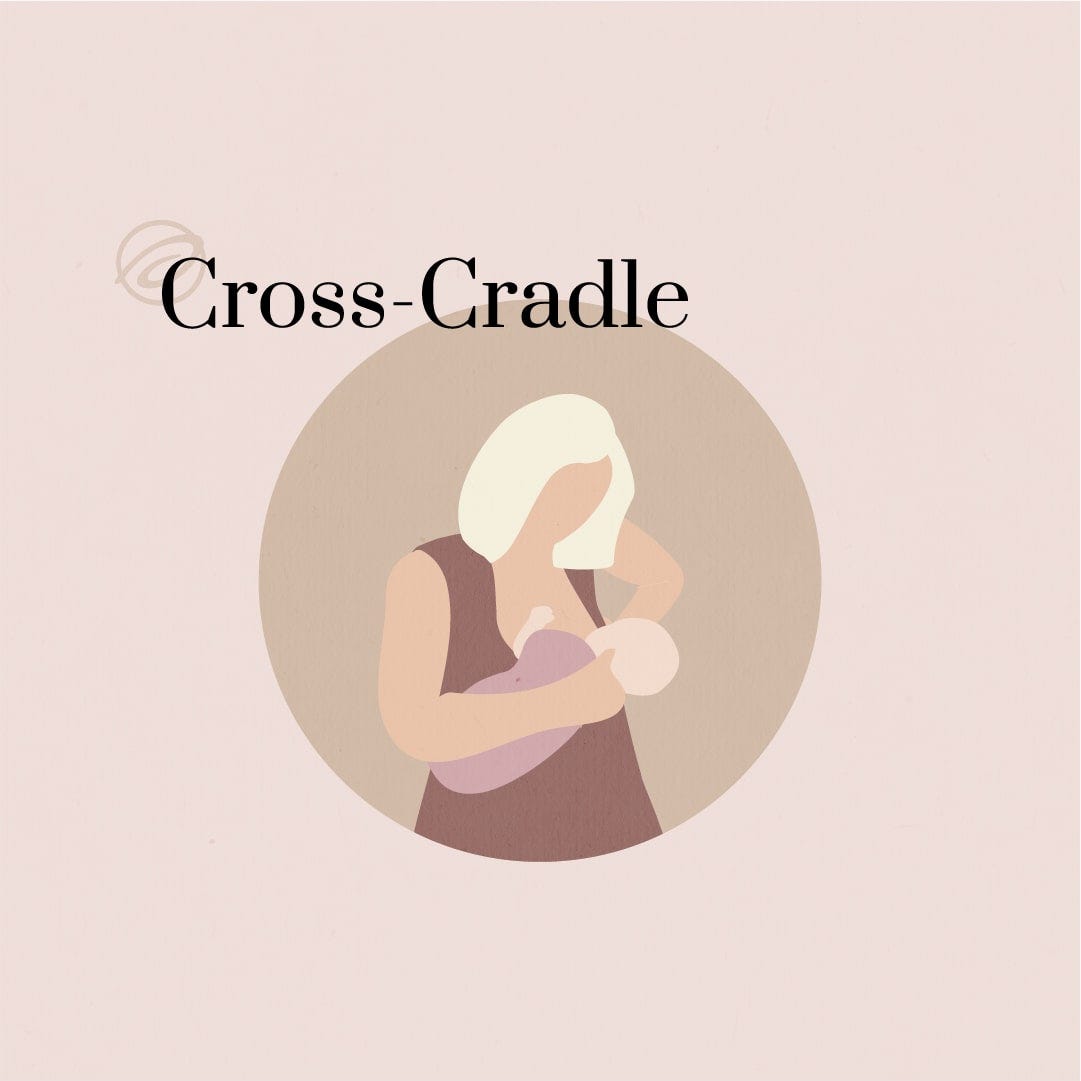
Cross-Cradle Hold
The cross-cradle looks similar to the cradle hold, but it allows the baby to feed from your opposite breast. In the cross-cradle, your baby’s body rests along the forearm/elbow opposite from the latching breast.
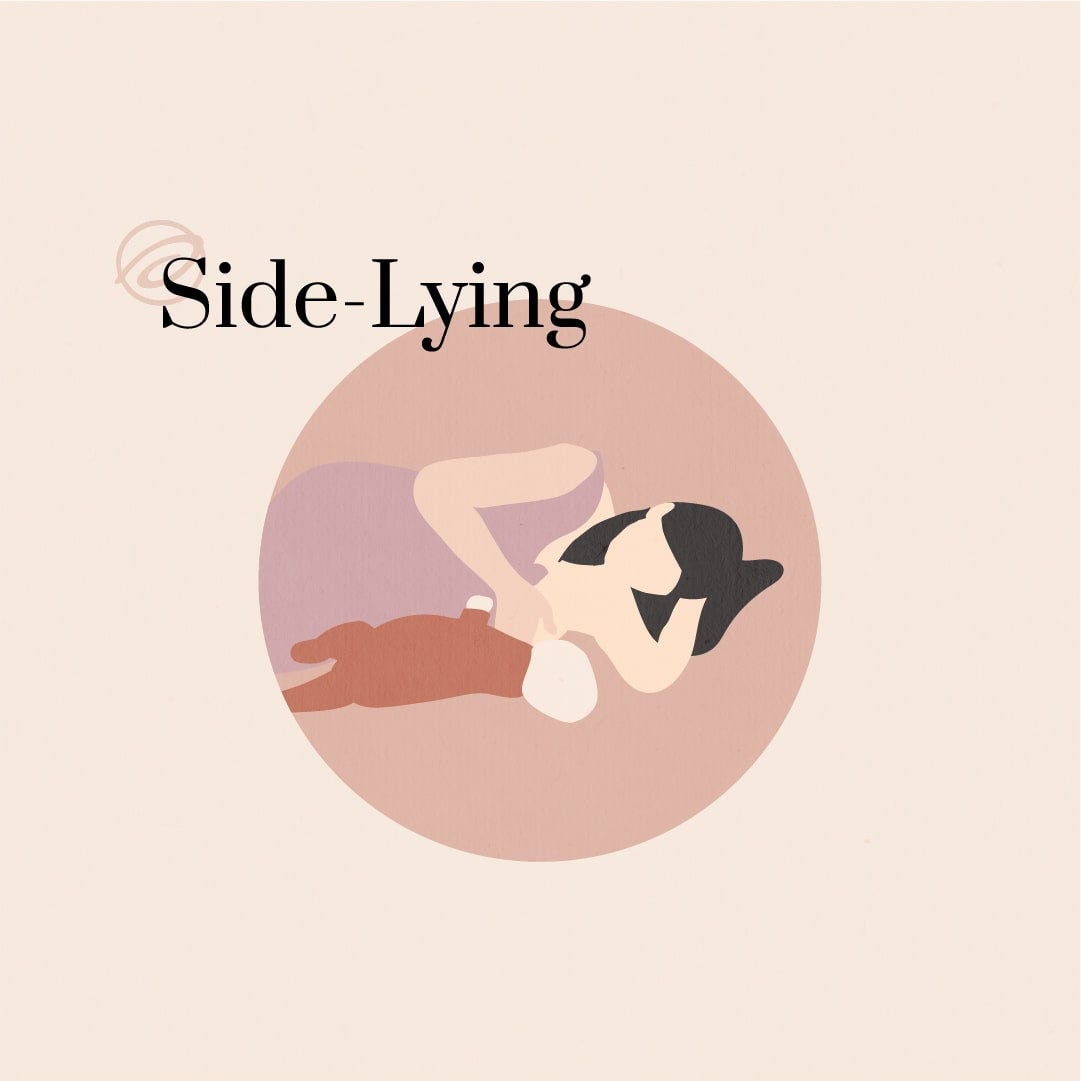
Side-Lying Hold
The side-lying position is often the most restful and comfortable for those who have just had a C-section. It allows you to lie in a comfortable position on your side without supporting your baby’s weight—the bed or sofa you’re lying on does the hard work for you.
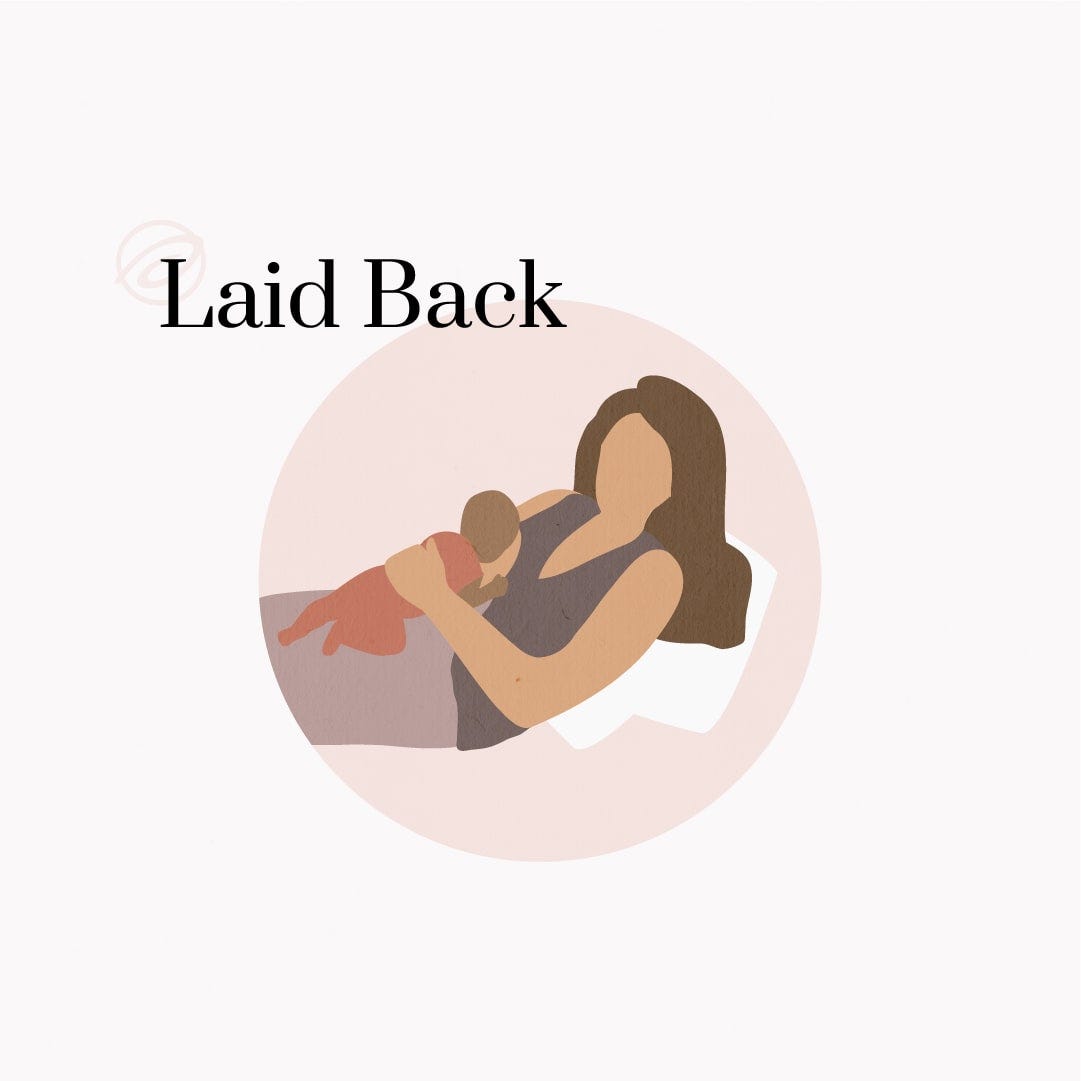
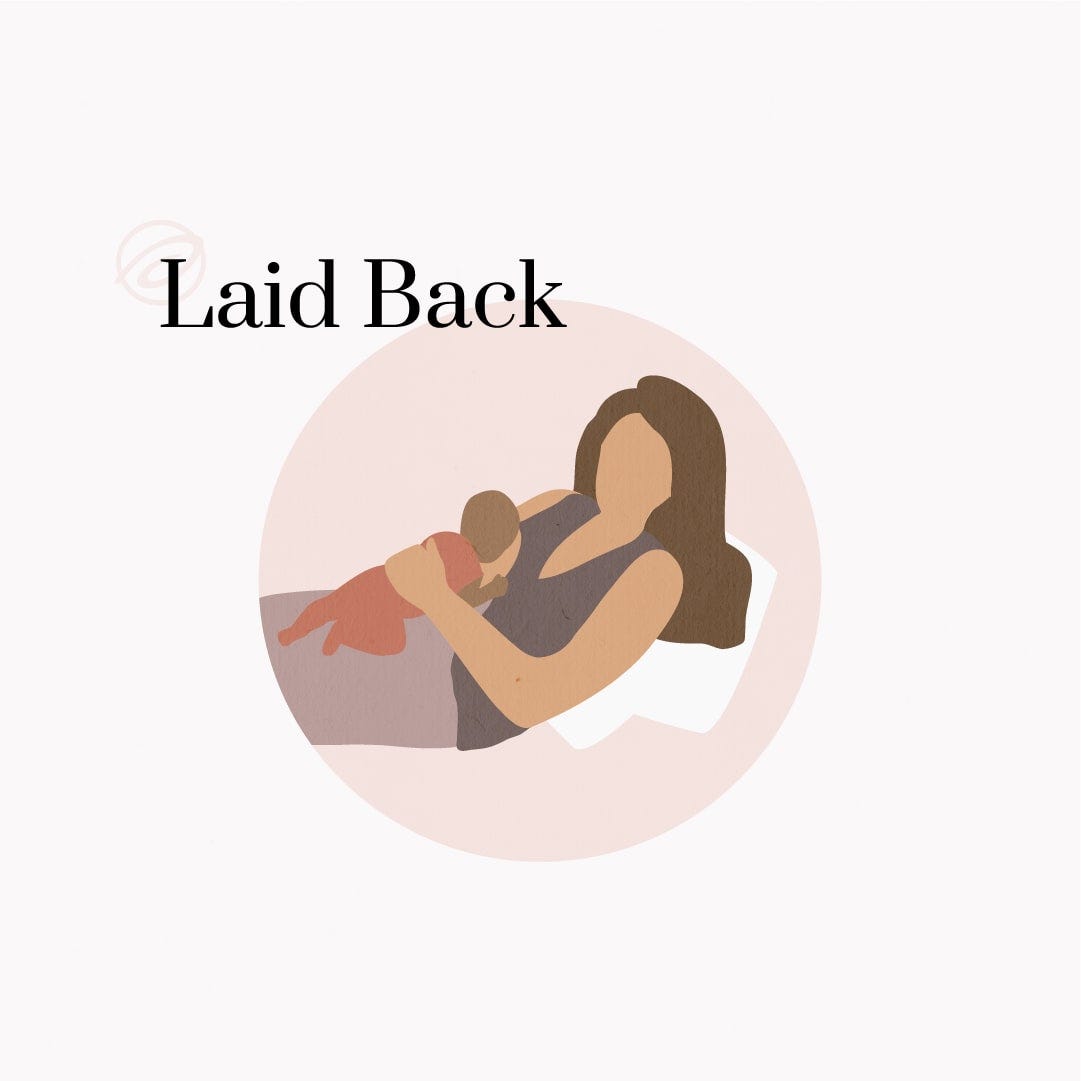
Laid Back Hold
This is another restful recovery position for people who have just had a C-section. Lay back on an angle, supporting your back with pillows. Your baby can rest on your upper belly and lower ribs to prevent pressure on your wound site.
Remember: there are no right or wrong breastfeeding positions! Do what works best for you and your little one, and remember to rest!
References
https://www.cdc.gov/nchs/data/nvsr/nvsr72/nvsr72-01.pdf
https://www.mayoclinic.org/diseases-conditions/placental-abruption/symptoms-causes/syc-20376458
https://www.mayoclinic.org/healthy-lifestyle/labor-and-delivery/in-depth/vbac/art-20044869
https://medlineplus.gov/ency/patientinstructions/000624.htm
https://www.nhs.uk/conditions/caesarean-section/recovery/
https://www.stgeorges.nhs.uk/wp-content/uploads/2021/09/Scar-scar-massage.pdf
https://www.marchofdimes.org/taxonomy/term/97
https://onlinelibrary.wiley.com/doi/full/10.1111/srt.13272