Sometimes, healthcare providers suggest starting labor before it begins on its own. This is called induction. While induction refers to starting labor, augmentation means giving your labor a boost when it has already started but has slowed down or isn't progressing as quickly as expected.
The idea might come up casually at an appointment:
-
“We can schedule your induction at 39 weeks.”
-
“You’re full term now; there’s no reason to wait.”
-
“Your baby looks big—let’s not take any chances.”
It's important to know that not all inductions or augmentations are medically necessary. Factors such as your health and your baby’s well-being influence the decision about whether to start or speed up labor. This is a time for you to ask questions, advocate for yourself, and make sure you understand why your healthcare provider might recommend either option—so you can make an informed decision.
Due Dates and Expectations
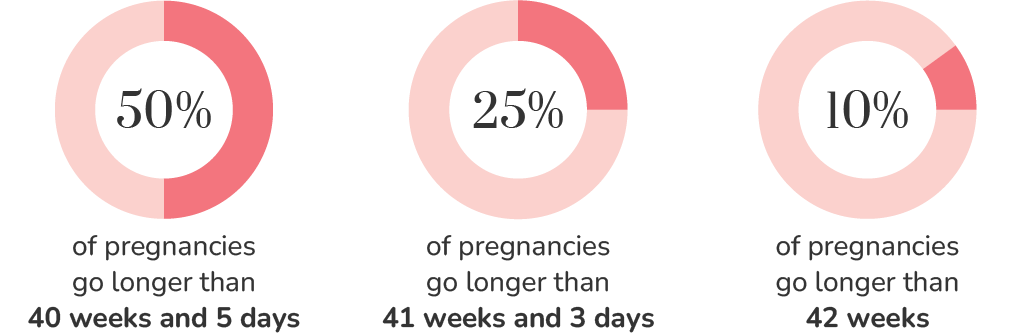
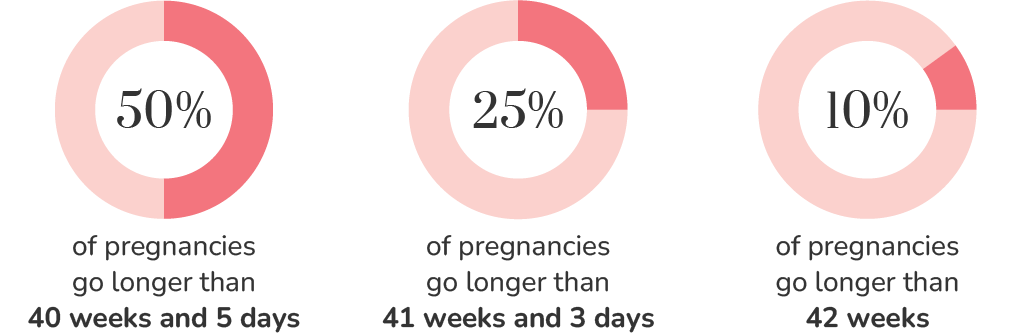
Decisions about induction often come up near or after your due date. Waiting can feel stressful, but it’s normal for labor to begin later than expected, especially in a first pregnancy. Research shows:
-
Only about 5% of babies are born on their exact due date.
-
For first-time moms (without induction), the average arrival is about 8 days after the due date—that’s 41 weeks and 1 day.
-
50% of pregnancies go past 40 weeks + 5 days.
-
25% go past 41 weeks + 3 days.
-
10% go past 42 weeks.
Your body knows what it’s doing. Those final days or weeks can feel long, but they’re often part of a normal, healthy pregnancy.
Reasons for Induction and Augmentation
Understanding why your provider may recommend induction or augmentation can help you feel more confident about your options:
-
Medically necessary: Sometimes induction or augmentation is recommended when there are health concerns such as high blood pressure, low amniotic fluid, or signs that continuing the pregnancy could pose risks to the baby’s or mother’s well-being.
-
Preventive or precautionary: Some providers may suggest routine induction around 39 weeks to lower the chance of certain complications that may develop later in pregnancy, even when both you and your baby are currently healthy.
-
Elective: In some cases, induction of labor is chosen for personal reasons or convenience, such as scheduling around work, childcare, or family plans.
What are medical indications for an induction?
-
Health issues such as heart, lung or kidney problems with mom
-
Diabetes (gestational diabetes or diagnosed before pregnancy)
-
Placenta concerns (such as placenta previa)
-
Restricted or poor fetal growth
-
Uterine infection
-
Chronic problems wth high blood pressure
-
Water breaks before labor begins
-
Approaching 2 weeks beyond due date and labor has not started
What are NOT medical indications for an induction?
-
"Big Baby" in an otherwise healthy pregnancy
-
"Induction at 39 weeks is always safe"
-
"Pregnancy after 40 weeks is dangerous"
-
Mom is tired of being pregnant
-
Wanting to pick baby's date of birth
-
Healthcare provider/hospital scheduling conflict
-
IVF
-
Geriatiric pregnancy or age 35 at delivery
-
Short or petite mothers
Options for Labor Induction and Augmentation
If you are having an induction or your labor needs to be augmented, your care team will closely monitor both you and your baby to ensure safety. This may include:
-
Continuous electronic fetal monitoring: Tracks your contractions and how your baby is tolerating labor.
-
IV fluids: Keeps you hydrated and allows easy access to administer medication, but may limit mobility.
-
Frequent blood pressure checks: Ensures your body is responding safely to medications and labor.
These monitoring and safety measures set the stage for the specific induction or augmentation methods your provider may use:
Stripping or Sweeping the Membranes
Gently sweeping the membranes during a cervical check can release natural prostaglandins to help soften the cervix and sometimes trigger contractions within a few days.
Prostaglandin Medications
These medications help soften or “ripen” the cervix. Options include:
-
A vaginal insert, such as Cervidil
-
A small tablet, such as Cytotec, taken orally or placed near the cervix
Breaking Your Water
A hook-like instrument is used to break the amniotic sac (bag of waters). As the fluid drains, the baby’s head presses on the cervix, which can help it thin and open, starting or speeding up labor.
Cervical Balloons (Foley Bulb)
A small balloon is inserted into the cervix and gently inflated to encourage dilation without medications.
Pitocin (Synthetic Oxytocin)
Administered through an IV to stimulate contractions after the cervix is ready. Dose is increased gradually until a good contraction pattern is achieved and can be adjusted or stopped if needed.
B.R.A.I.N. Questions to Ask Your Healthcare Provider
B.R.A.I.N. stands for Benefits, Risks, Alternatives, Intuition, and Nothing (time to decide)—a helpful framework to guide conversations with your provider. Questions to consider:
-
Why are you suggesting induction or augmentation?
-
What is my Bishop Score? (This test shows how likely it is that your cervix will dilate and labor will progress.)
-
What medication or instruments will you use and what are the possible side effects to me and my baby?
-
What are my options if it doesn't work?
-
How long will you try induction before recommending a cesarean?
-
What can I do to try to start labor naturally in the meantime?
How Can Induction or Augmentation Affect Breastfeeding?
Some birth interventions, including induction or augmentation, can temporarily affect your baby’s alertness or your comfort with breastfeeding in the early days. This is normal, and most mothers are able to overcome early challenges and go onto successful breastfeeding with the right support.
Potential Challenges You Might Notice
For you:
-
Feeling exhausted after a long or intense labor: Take advantage of skin-to-skin time while resting, and accept help from your partner, family, or nurses to bring the baby and assist with breastfeeding.
-
Engorgement from IV fluids: If your baby is struggling to latch, hand express a small amount of milk to relieve discomfort and help your baby latch more easily.
-
Limited mobility if you had an epidural or cesarean: Use pillows to support positioning and experiment with different feeding positions, such as side-lying or football hold.
-
Possible delayed milk production: Some women may notice that milk “comes in” a little later after induction or augmentation. Frequent milk removal (breastfeeding or pumping) can support you supply.
For your baby:
-
Sleepiness: Pain medications, epidurals, or synthetic oxytocin may make babies a little drowsier in the first hours after birth. This is usually temporary and resolves within the first day or two.
-
Reduced alertness for feeds: Offer skin-to-skin contact frequently to encourage alertness and rooting. Gently wake your baby for feedings every 2–3 hours if they are not waking on their own.
-
Difficulty latching or suckling effectively: Some babies need extra support with feedings, so getting started with additional milk removal will help ensure they receive enough milk.
-
Slightly higher risk of jaundice: Babies born after induction or augmentation may have an increased risk of mild jaundice, necessitating monitoring and possibly treatment.
-
More noticeable early weight loss: Babies born after induction or augmentation may lose more weight in the first few days due to extra fluids given during labor. This can temporarily exaggerate weight loss and impact parents’ confidence in feeding.
After an induction you may:
- Be tired, especially if the birth was long or difficult
- Engorgement from IV fluids
- May have limited mobility if you received an epidural or had cesarean birth
After induction your baby may:
- Be sleepy
- Have difficulty latching
- Have difficulty suckling
Supporting Successful Breastfeeding
-
Keep your baby in your room with you 24/7 and hold them skin-to-skin as often as possible.
-
Practice exclusive breastfeeding after birth, feeding on cue at least 8-12 times per day.
-
Track your baby's wet and dirty diapers to ensure they are getting enough milk.
-
If your baby struggles to latch, initiate hand expression and offer expressed breast milk with a spoon, cup, or syringe.
-
If you and your baby are separated, use a breast pump every 3 hours, even at night, to stimulate milk production until they are able to breastfeed directly.
-
Be patient and remember that babies need time to establish a rhythm and feeding patterns can vary widely in the first days.
Every birth and breastfeeding journey is unique, and early challenges after induction or augmentation are usually temporary. By understanding what to expect—from your own recovery and energy levels to your baby’s alertness and feeding patterns—you can feel more prepared, confident, and patient as you and your baby find your rhythm together.
Disclaimer: Our classes and accompanying materials are intended for general education purposes and should not replace medical advice. For personalized recommendations, please consult your healthcare provider and/or lactation consultant.




More Pregnancy Care Guides
Maternity Bag Essentials
Preparing to Breastfeed After Surrogacy or Adoption
How Taking Antibiotics During Birth Can Influence Breastfeeding Outcomes
How Placenta Encapsulation Can Influence Breastfeeding Outcomes
Nutrition During Pregnancy