One of the typical worries during lactation is getting a clogged milk duct. Horror stories abound about hard, painful, tender lumps, the lengths people go to get rid of them, and what can happen if they don’t resolve. Luckily, clogged ducts are not as common as you may think, and recently much more about them has become clear. Many mothers have thought that they had a clog, which turned out to be a normal full duct. If you feel something hard and prominent before nursing or pumping, but is gone afterward, there is nothing to worry about!
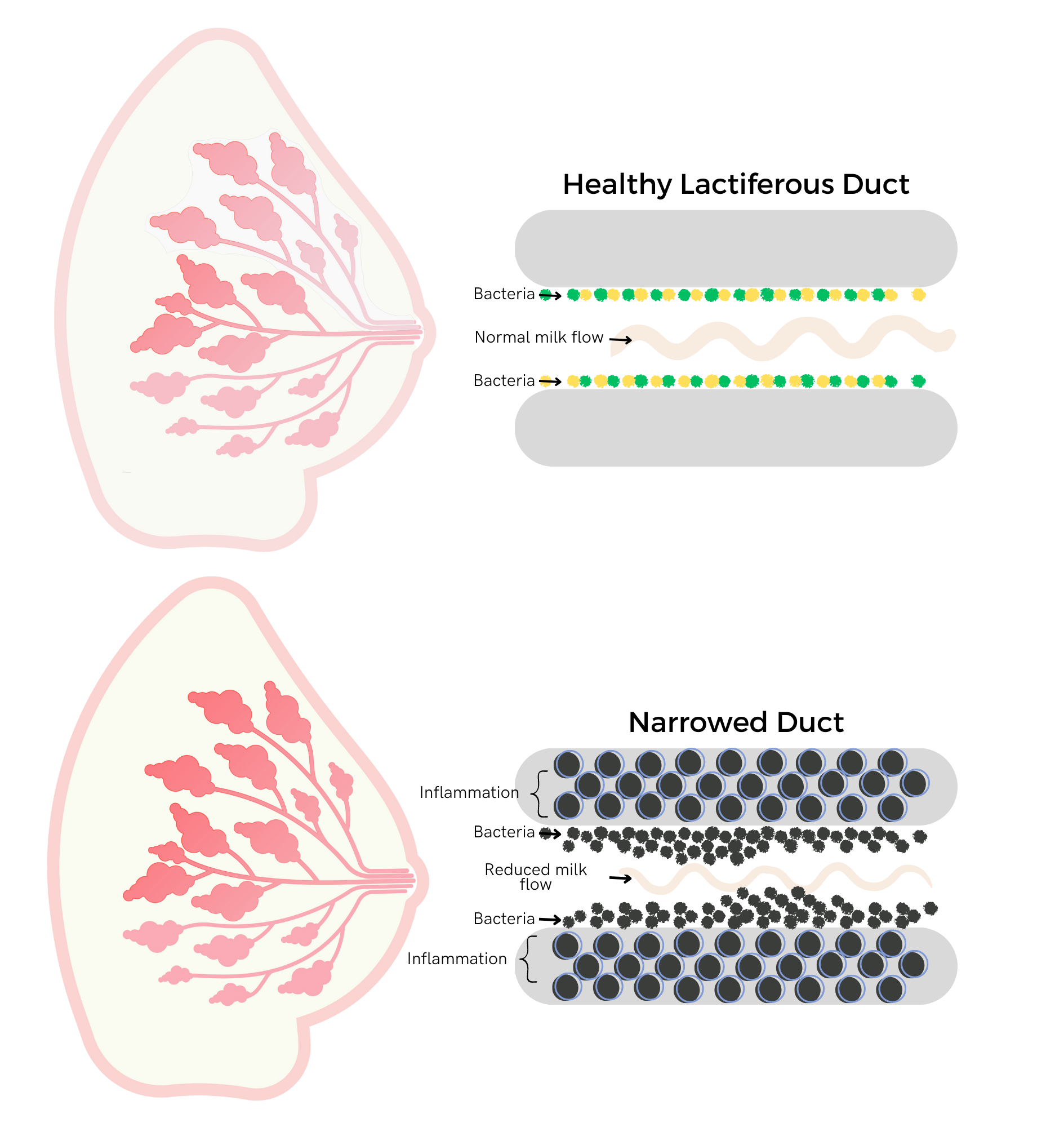
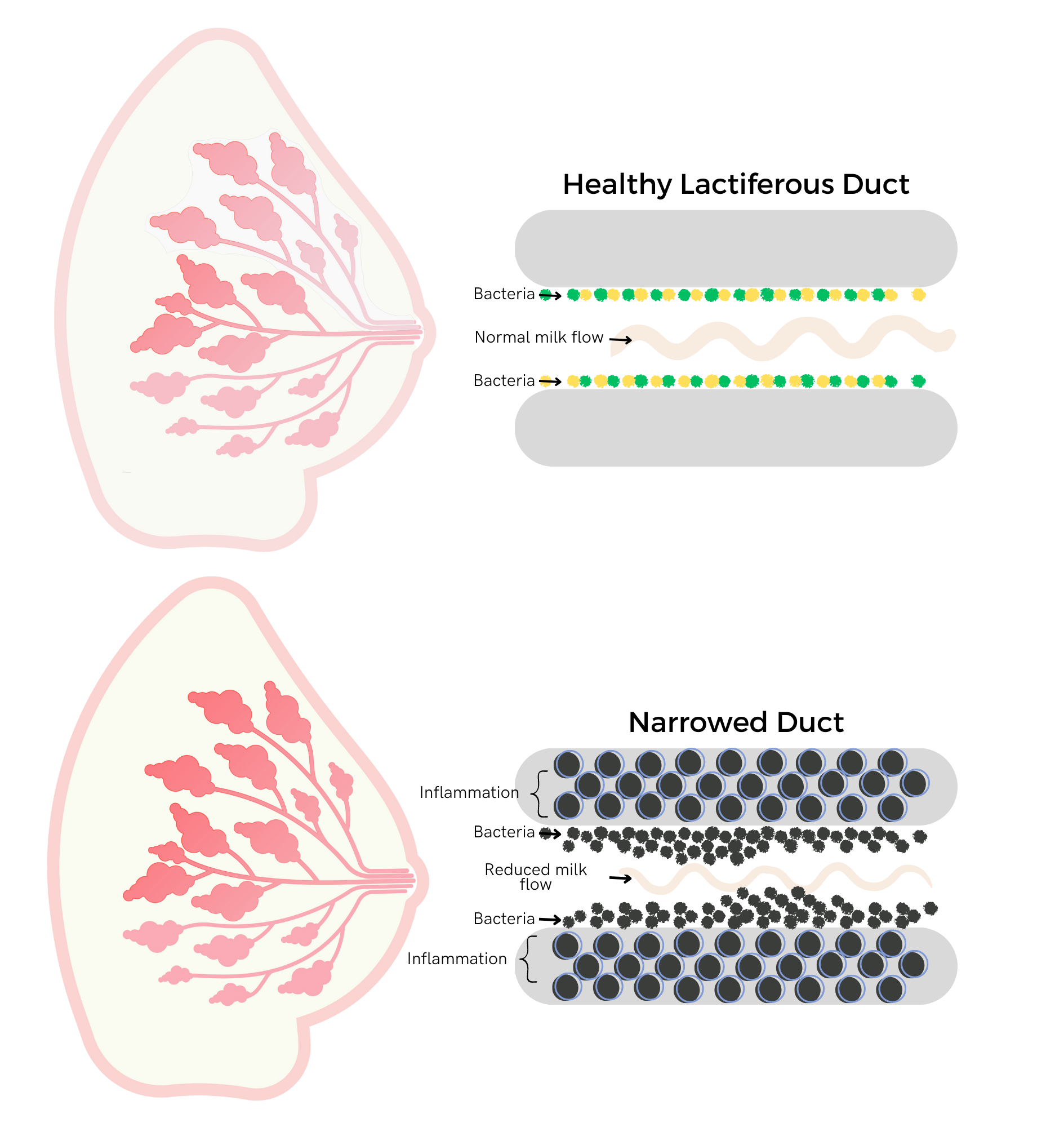
A more accurate term than “clog” or “plugged milk ducts” that has come into use among lactation and health professionals is ductal narrowing. Research has shown that, contrary to popular belief, true clogs of sticky or dried milk don’t actually exist. Even though a painful area on the affected breast can be felt externally with fingers, or perceived internally, it is actually an area of narrowed milk ducts and the swelling of surrounding tissues. It is the same concept of a sprained ankle – the injury is to the ligaments, but the tissues in the immediate area all become swollen in response.
What Can Cause Inflammation That Leads To Ductal Narrowing?
Many factors influence levels of inflammation in our bodies including diet, health conditions, and genetics. However, two common causes of inflammation leading to ductal narrowing are hyperlactation (oversupply) and an overgrowth of certain bacteria and biofilm which is called mammary dysbiosis. The issue isn’t a blockage or blocked milk ducts; it stems from too much milk trying to navigate pathways that are diminished by extra cells, causing it to slow and eventually stop. It’s like a traffic jam in the duct with too much milk (the cars and trucks) for the narrow ducts (roads with lane closures).
Unfortunately, many mothers are given well-meaning advice from friends about pumping early on to create a stash of breast milk in their freezer. While satisfying and confidence-inspiring, especially for those planning to return to work, overstimulation early on can create an oversupply and engorgement. Too much milk can be uncomfortable for the mother and can create a forceful milk ejection and fast flow of milk for baby when feeding at the breast. Babies can become gassy, unsettled and spit up larger volumes. Additionally, a constant state of oversupply puts mothers at risk for ductal narrowing, mastitis, breast infection, and more. Ideally, the baby should be fed on cue with no extra milk being expressed in the early weeks. This helps to ensure the right amount of milk for a good supply – not too little or too much.
When babies begin to sleep for longer periods of time, many mothers think they need to breast pump to replace the feeds that the baby is sleeping through. This is not necessary. The baby has adapted and changed their sleeping pattern, and the breasts will follow. There may be fullness or even discomfort for a few days as they adjust, but leaving things alone to settle is the best policy. If there is a lot of discomfort, it’s fine to remove a small amount of milk just to help you get to the next feeding more comfortably. However, if you decide to empty your breasts thoroughly, you are sending the message that the milk is needed, so more will be made. Some mothers like this idea initially as the thought of having a full freezer is appealing. In time, when they find themselves pumping alone in the middle of the night as everyone else sleeps, it can seem like less of a great idea! Your milk supply will go through increases and decreases as your baby grows and develops. It is designed to do this, so just go with the flow!
New Information
More and more attention is being given to maintaining a healthy biome throughout the body where good bacteria is abundant and keeps problematic bacteria in check. This is also true for the breast and human milk biome. Eating to support a healthy biome, not routinely cleaning your nipples (apart from bathing every day or so), and not sterilizing pump parts are all important preventive measures. In past generations, emphasis was placed upon hyper-cleanliness for babies’ areas, items, and caregivers. However, babies need access to the typical bacteria, fungi, and viruses in their world. Their immune system has to learn and develop- and does so by normal interaction with these organisms. Too much cleaning wipes out the good and the bad bacteria which is a hindrance. We also now understand the importance of the “good” bacteria and how too much cleaning and sterilizing disrupts the balance in our bodies.
An Ounce of Prevention
The best way to avoid problems with ductal narrowing is to be sure that milk can keep moving freely. Here are some tips:
- Learn about breast anatomy and lactation physiology.
- Do your best to eat a healthful diet.
- Feed on cue without a goal of “emptying the breasts.”
- If using a pump, only remove the amount of milk that the baby will eat.
- Ensure good flange fit and comfortable suction level to avoid injury to the nipple/areola.
- Avoid sleeping while wearing a bra, or tight straps from a bag, backpack, or baby carrier worn for long periods of time.
- Avoid nipple shields as they can impede milk removal.
- Ensure that bras fit appropriately and don’t restrict milk flow.
- Remove tighter sports bras or exercise clothing as soon as possible after finishing your workout.
- Do not deeply massage breasts, use vibrating devices, or roughly hand express milk.
- Get help from an IBCLC for breastfeeding support and to address oversupply.
Inaccurate And Outdated Advice On The Internet Lives Forever
One popular internet recommendation is to fill a silicone “pump” or milk catcher with warm water and Epsom salts. While the warmth may offer temporary comfort, the heat can make inflammation worse and saline soaks can macerate the skin. Additionally, this technique is not effective on the deeper areas of the breast likely to be affected.
In recent years, vibrating “massagers” have been marketed and sold to parents with the promise of helping to relieve clogs. Prior to the arrival of these specific devices, the advice was to apply an electric toothbrush, toy, or anything else on hand that vibrated to the affected area. We know now that extended periods of firm pressured massage and strong vibration only make inflammation worse.
Most internet searches still yield outdated and potentially harmful advice about aggressive treatment with lots of heat, deep massage, pumping, “draining the breast,” etc.
Recurrence and Complications
If you have an area that seems “clogged” and won’t resolve, or if additional symptoms appear (especially flu-like symptoms), it is best to seek help from an IBCLC. Concerning symptoms include: fever, body-aches, increasing pain, a warm, painful area on the breast, an increase in the size of the affected area, and color changes or streaks on the skin of the breast. For people with darker skin tones, the skin may appear darker brown, purple, red, or have streaks. Lighter skin-toned people may see red or pink skin or streaks.
It is possible for ductal narrowing to worsen and become mastitis or other conditions. Ideally, addressing issues quickly and appropriately will help avoid further problems.
For recurring issues, addressing oversupply and promoting a healthy breast biome are crucial. Additionally, there is research to support taking a sunflower or soy lecithin supplement to help prevent future problems by reducing inflammation in ducts and better emulsifying milk.
If You Suspect a “Clog”
Do:
- Feed or remove milk based on the baby’s actual needs and cues and not more.
- Use cool compresses to soothe discomfort right after or in between feedings. Warm compresses are only OK for a few minutes immediately before feeding or removing milk.
- Ask your healthcare provider about a regimen of acetaminophen and ibuprofen to address inflammation and discomfort.
- Try gentle lymphatic drainage massage with light sweeping of the skin from the nipple towards the clavicle.Know that therapeutic ultrasound can be a good option for relief.
- Consider taking a sunflower or soy lecithin supplement (5-10g per day).
- Consider taking a probiotic supplement specific to lactation support.
- Reach out for help from an IBCLC
Don't:
- Panic. You’ve got this!
- Overstimulate milk production.
- Use hot compresses.
- Massage the breast tissue deeply or aggressively, or use vibration devices.
- Use saline soaks or castor oil compresses.
- Use underwire bras, tight bras, or other tight clothing.
What If I Have Questions?
If you are interested in learning more about ductal narrowing and breastfeeding, you can schedule a one-on-one appointment with an Aeroflow lactation consultant here.
References
Johnson, H., Eglash, A., Mitchell, K., Leeper, K., Smillie, C., Moore-Ostby, L., Manson,
N., Simon, L. & the Academy of Breastfeeding Medicine. (2020). ABM clinical protocol #32: Management of hyperlactation. Breastfeeding Medicine, 15(3): 1-6.
Mitchell, K., Johnson, H., Rodriguez, J., Eglash, Scherzinger, C., Zakarija-Grkovic, I.,
Cash, K., Berens, P., Miller, B. & the Academy of Breastfeeding Medicine. (2022). Academy of Breastfeeding Medicine clinical protocol #36: The mastitis spectrum, revised 2022. Breastfeeding Medicine, 17(5): 360-376.









