A Beginners Guide to Breast Pumping
If you’re ready to master the art of breast pumping then you’ve come to the right place. As a new or expectant mother you’ve got enough to worry about, and how to use your breast pump shouldn’t be one of them. That’s why we’ve broken down pumping to an exact science to help you learn all of the dos and don’ts!
Do I Need A Breast Pump?
No, but they certainly help and it’s a required benefit so you’re insurance will cover a breast pump.. Breast pumping can be beneficial for a variety of different situations:
- They can relieve engorgement and prevent mastitis.
- They allow you to provide breast milk when nursing isn’t an option due to latching or other complications.
- Pumps give your partner or other caregivers the ability to help out with feedings and enhance bonding with baby.
- They help you build and maintain an adequate milk supply.
- They allow you to run a quick errand or participate in date night because you can be away from baby for a few hours without missing a feeding.
- They make it easier to maintain your breast pumping goals by providing the ability to pump once you return to work.
- Many women enjoy the convenience of breast pumping on the go. Some options weigh less than a pound, so you can throw it in a bag and go! Plus, battery-powered options can be used to pump when no other power sources are available!
The Benefits Of Breastfeeding
Research has shown that breastfeeding is extremely beneficial for the health of both mom and baby, especially when you exclusively breastfeed for at least six months.
Benefits for baby:
- Breast milk is full of naturally occurring nutrition for your baby, including vitamins, proteins, and fats that provide everything needed to grow healthy, big, and strong. Plus, it’s much easier to digest than formula.
- Your milk also contains antibodies to help your baby fight viruses, bacteria, illnesses, and diarrhea. Breastfed babies are often healthier and require fewer trips to the doctor with a reduced risk of developing asthma, allergies, diabetes, and obesity.
Benefits For Mom:
- Breastfeeding releases oxytocin, the hormone that can help reduce uterine bleeding and assist with returning your uterus to its normal size faster and giving birth.
- Because breastfeeding burns about an extra 500 calories a day it can help you burn fat to possibly return to your pre-pregnancy weight faster.
- Breastfeeding saves time and money! Instead of spending a ton on formula that you have to mix and heat up you can provide breast milk to your baby for free, straight from the boob!
How Do Breast Pumps Work?
If you feel as breast pumps work in mysterious ways as intricate medical devices, don’t worry Mama. You’ve got this. They’re actually pretty easy to assemble and use.
- A breast pump emulates a nursing baby by mimicking their natural suckling pattern. As infant nurses, he/she doesn't apply constant pressure to the breast. The average baby sucks about 50 to 90 times per minute, and slow down once milk is released. An electric breast pump will create this cycle of suction and release by producing one pull per second to initiate milk let down as breast milk begins to flow.
Breast pump suction mirrors baby’s natural sucking through several phases:
Let Down - mimics when baby is vigorously sucking. This phase stimulates the nerves in your breasts, which signals the release of a hormone called oxytocin. The release of oxytocin will make the small muscles that surround your milk-producing tissue to contract, which squeezes milk into your ducts.
Expression - mirrors when baby's sucking slows down, and he/she is swallowing milk. This is sometimes called "suck, pause, swallow."
Leah DeShay, CLEC, IBCLC
- As breast milk is expressed from the breast it collects in a storage container. The containers are gravity fed so the milk that’s released drips downward into them.
- Breast pumps come with flanges, also known as breast shields, which are funnel-shaped plastic parts that are placed over the nipple and areola to create a seal. The nipple is gently pulled into the flange tunnel to release milk. Make sure you have the correct flange size for pumping success.
Does Breast Pumping Hurt?
It can, but it shouldn’t. The first 10 to 15 seconds may be uncomfortable as your nipples begin to stretch and your milk begins to flow, but that generally takes a bit of getting used to. If you experience pain, soreness, or chaffing you may need to:
Change your flange size. If your flange is too big or too small it can pinch the sides of your nipple and pull the areola inside of the tunnel.
Change positions. Make sure that your nipple is in the center of your flange. If it’s off to one side it can get pulled and pinched in the flange tunnel.
Adjust the speed and suction settings. If the suction strength or speed is too high, it may cause irritation and discomfort. The highest settings are much stronger than an infant’s natural suckling pattern.
Don’t over pump. It takes the breasts about 15 to 30 minutes to empty. Do not pump for more than 30 minutes. If you’re having trouble getting your milk to flow try using a warm compress or massaging your breasts prior to pumping.
Using a pump should be a similar sensation to comfortable breastfeeding: some pressure and gentle tugging. If you catch yourself dreading the feeling of your pumping sessions or wince while pumping, its is, quite literally, counterproductive to ignore.
How To Set Up Your New Breast Pump
Once you receive your breast pump through insurance don’t feel overwhelmed once you open the box to find tubing, small parts, and bottles! We believe in you Mama, setting your pump up is easy with just a few simple steps
- Don’t wait til baby arrives to set up your pump. After your delivery, you don’t want to have to worry about setting your pump up. Take about an hour before your due date to put your pump together and to become familiar with how to use it.
- Bust out that instruction manual to learn about how to use your pump. Follow it’s directions and store it somewhere safe. Your pump manual might have resources for troubleshooting your pump if issues arise. Plus, YouTube is another great resource for learning how to put pump parts together. Some manufacturers have educational videos as well.
- Sterilize your breast pump parts before use. Check to see if your breast pump is dishwasher safe before placing parts in there. Usually, its recommended to remove breast pump parts from the dishwasher before the drying cycles, as it can warp the parts.
- Some people prefer to boil their breast pump parts in water for about five minutes.
- Medela makes steam bags that allow you to sterilize your pump parts in a matter of minutes in the microwave.
- After your breast pump has been sterilized allow the parts to completely air dry before storing them or putting the parts together.
If you have a closed system pump do not worry about cleaning the tubing. However, it is recommended to clean your tubing with an open system breast pump. - Take your time. Be patient. Learning can take a little time, that’s why it’s important to get started before your little bundle of joy arrives. Most pumps have a variety of suction settings and pumping cycles to become familiar with. While it’s recommended to try on your flanges before your baby is born to make sure they fit, it’s not recommended to try your pump out.
- Plan ahead with breast pump accessories. The breast pump is only the tip of the iceberg! Accessories such as nursing pads, a breast pump tote bag, hands-free bra, or nursing pillow cold all be added to your registry as essential items to make expressing milk easier and more comfortable.
How To Use A Breast Pump
Now that you know how to pick a breast pump let’s tacking how to breast pump. The process is simple, but it can take some getting used to.
When do I start pumping after birth?
After giving birth you can either start breast pumping right away (one to six hours afterward) to provide for your infant. If they don’t have issues latching you can actually breastfeed them and wait a few weeks prior to pumping.
- Start breast pumping when you’re ready to build and/or store a supply of breast milk to provide your baby with. Then remember to stick to your pumping schedule to keep your milk supply consistent.
Sleep is a big topic for new parents. During the first month, you can begin using your breast pump to store milk in order to give your partner the opportunity to feed the baby during the night. This can help your partner have bonding time and share the responsibilities of midnight feeding. It will also give you a chance to practice setting up and using your pump.
- If you’re returning to work, try to start pumping a few weeks (if you have that amount of time) before you return. Waiting until the day before might be stressful and frustrating.
- Pump in the morning, that's when moms tend to get the most milk.
- Pump between feedings, either 30 to 60 minutes after nursing or an hour before breastfeeding. This will leave plenty of milk for baby during the next feeding.
- It’s fine to breastfeed right after pumping, some babies are patients and will feed longer to get the milk they need.
To properly breast pump refer to the following instructions:
- Bust out that instruction manual to refresh your memory on to properly use your pump and to take note of any special features. But generally pumping is as easy as:
- Placing the breast shield on your nipple, and
- Turning your electric pump on, or squeezing the mechanism if your pump is manual. - Relax. Find a comfortable place to pump that's free from distractions. Make sure your shoulders are back and your arms are supported. Applying a warm compress to your breasts can enhance let down, the process when your milk begins to flow. Massaging your breasts before and after pumping can also help.
Don’t worry if it takes your milk several minutes before your milk begins to flow. Be patient, it’s not immediate at first.
Practicing pumping before you need milk can help your body get used to your pump so you’ll be more comfortable with the process.
- Stick to a breast pumping schedule. Pumping at the same times each day can help your body produce more milk as demand increases. Also, looking at a picture of your baby or listening to them can help stimulate more milk.
If you’re exclusively pumping them make sure you pump more frequently to store enough milk for your infant. If you’re breastfeeding and pumping, pump about 30 minutes after feeding your baby or 60 minutes before.
- Clean your equipment as directed, as soon as you can after uses. Wash all of your equipment with warm soapy water and let them fully air dry.
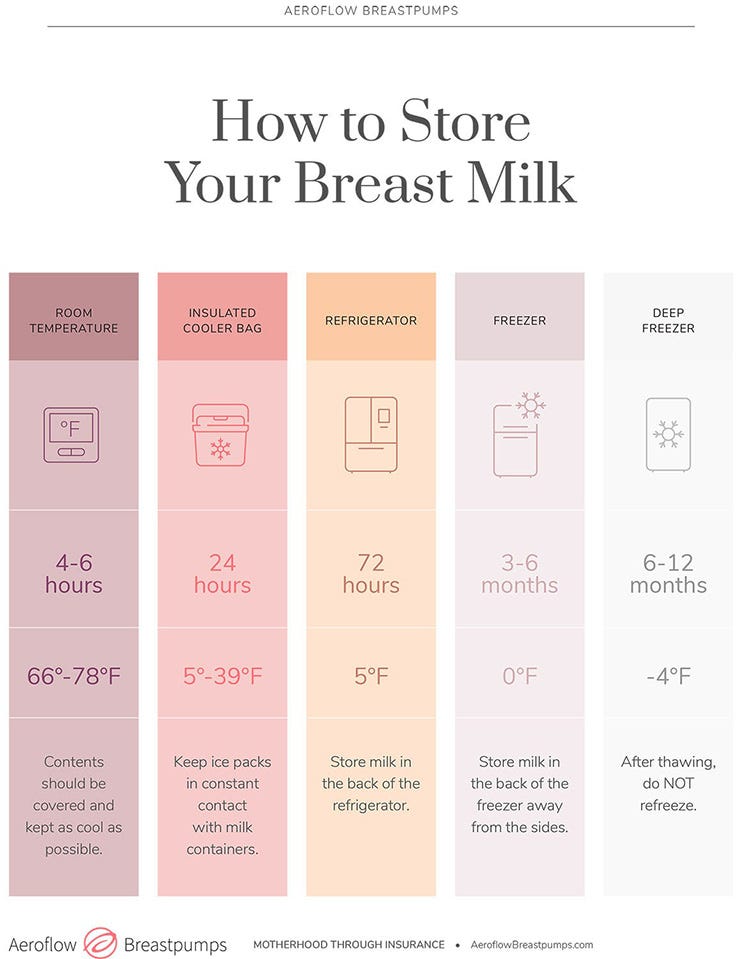
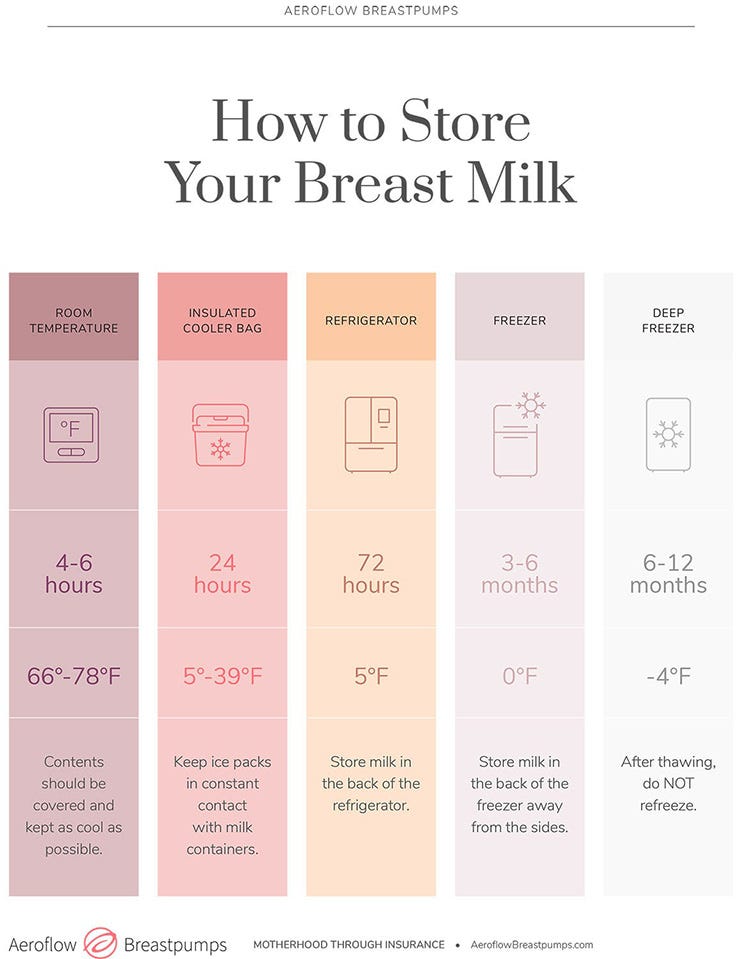
- Store your milk properly by labeling the date the milk was expressed storage container with a waterproof marker. Only use breast pump storage bags for freezing milk. Place the container in the back of the fridge or freezer so it’s temperature will remain consistent.
- Breast milk can be stored in the refrigerator for up to five days.
- Breast milk will last for about six months in the freezer.
- Your milk will be fine for one day in a cooler.
- You can leave your milk out at room temperature for up to six hours.
How Often Should I Breast pump?
How often you breast pump depends on a few different factors such as if you want to build a bigger milk supply, if you’re exclusively breastfeeding, or if you’re going back to work and might be away from your baby regularly.
- If you plan to stay at home with your baby and you're available for breastfeeding, you may only need to pump occasionally. Early on, you should breastfeed or pump 8 to 10 times a day as your milk supply becomes established.
- Your breasts will make more milk when there’s a higher demand for it, so it’s important to breastfeed or pump regularly to boost your supply.
- If your baby feeds regularly and you only want to pump occasionally, it’s best to pump in the morning. It was also help to pump in between feedings, about 30 minutes after or 60 minutes before.
How Much Milk Should I Pump?
When breast pumping be sure to fully empty both breasts. This process could take 25 to 30 minutes. Continue breast pumping for a few minutes after the last few drops of milk have passed to make sure you're done.
The amount of breast milk you produce will vary based on your baby’s age, time a day, how often you pump or feed, the quality of your pump, diet, and more.
Based on your child’s age, you can expect to pump:
Days 5 - 7 - Up to 2oz.
1 to 3 weeks old - Up to about 3oz.
4 weeks to six months old - up to 5oz.
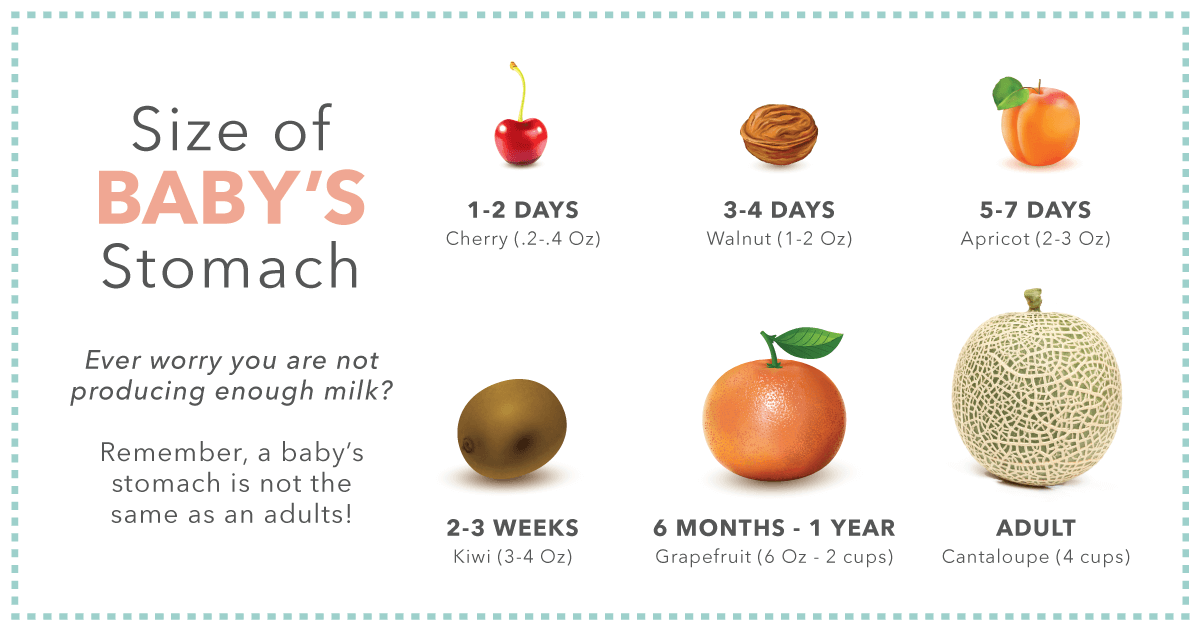
Don't worry if you aren't pumping very much breast milk during the first few days after your baby is born. Their stomach is still very tiny, so it's normal to only pump about 2oz during the first 5 to 7 days.
All moms are different! Some produce more milk and others produce less. If you’re concerned about your breast milk production, speak with your doctor or a lactation professional.
Bonus Breast Pumping Tips!
Once you get the hang of breast pumping, check out these times to make your life easier!
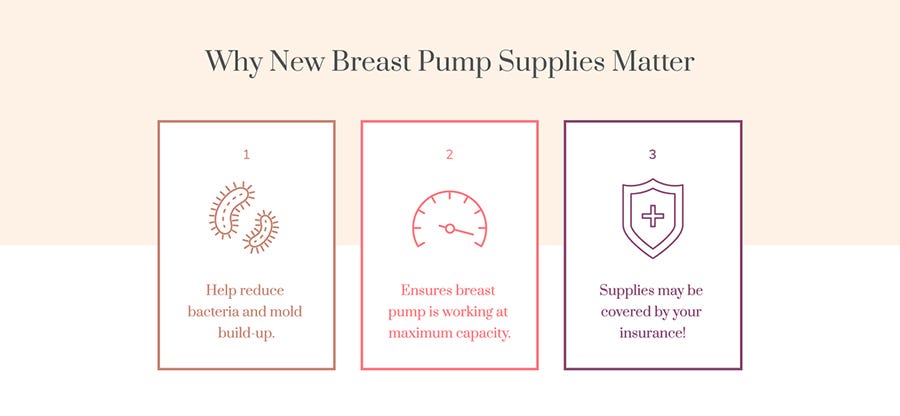
- Replace Breast Pump Parts
Your breast pump supplies need to be replaced on a regular basis to keep your pump functioning like brand new and you may qualify for replacement parts through insurance too!
Worn out breast pump parts are actually the number one cause of decreased milk supply. This is because worn out parts can lead to a decrease in breast pump suction.
- Let Down And More Milk
If you’re stressed out or at work with your flanges on and can barely get a single drop of milk try to relax. Save a TV show or book to enjoy only while you pump. Also, photos of your baby or something that smells like them can help produce more milk when you’re away from them.
Simulating the warmth of your baby’s mouth with a warm compress, a warm massage, or warm flanges can also increase your breast milk speed and out put.
Using breast massage and hand expression along with pumping with an electric breast pump is the best way to maximize milk output.
- Storage At Work
When you pump at work, where does your milk go?! You can put it in the fridge, but be sure to label it as yours. Also, separating your milk into smaller portions will help you save milk if your baby doesn’t drink a whole 8 oz.
If you don’t have access to a fridge at work keep your milk in an insulated cooler with ice or ice packs. Also, using milk storage bags that lay flat are easier for storing because they’re easier to stack.
- Travel And The Airport
Be prepared in the airport, mama. Have your pump ready to pull out of your carry on bag and place it in a separate bin for the x-ray machine. Tell the agent that you have a breast pump. As a medical item, it will not count as a carry-on. It’s best to have it in your carry one because you don’t want to be separated from your ump in the event of a delay or if your checked bag is lost.
You can take your breast milk on the plane in quantities higher than 3.4 oz. Tell the TSA agent that it’s breast milk, and be aware that they may need to test it with a swab.
Getting Your Breast Pump Through Insurance
If you're ready to master the art of breast pumping then you’ve come to the right place. As a new or expectant mother you’ve got enough to worry about, and how to use your breast pump shouldn’t be one of them. That’s why we’ve broken down pumping to an exact science to help you learn all of the dos and don’ts!
Do I Need a Breast Pump?
Do I Need a Breast Pump?
If you intend to provide breast milk for your baby and might be away for periods of time (like going back to work), you will need a breast pump. But you do not necessarily need a breast pump to breastfeed. Breast pumping can be beneficial in a variety of different situations:
- They can relieve engorgement and prevent mastitis.
- They allow you to provide breast milk when nursing isn't an option due to latching challenges or other complications.
- Pumps give your partner or other caregivers the ability to help with feedings and enhance their bond with baby.
- They help you build and maintain an adequate milk supply.
- They allow you to do other things that require you to be away from baby for a few hours without missing a feeding.
- They make it easier to maintain your breast pumping goals by providing the ability to pump once you return to work.
- Many women enjoy the convenience of breast pumping on the go.
- Some options weigh less than a pound, so you can simply throw your pump in a bag and go!
- Battery-powered options can be used to pump when no other power sources are available.
The Benefits of Breastfeeding
The Benefits of Breastfeeding
Research has shown that breastfeeding is extremely beneficial for the health of both mom and baby, especially when you exclusively breastfeed for at least six months.
Benefits for Baby:
- Breast milk is rich in nutrients for your baby, including vitamins, proteins, and fats that provide everything needed to grow healthy and strong. Plus, it’s much easier to digest than formula.
- Your milk also contains antibodies to help your baby fight viruses, bacteria, illnesses, and diarrhea. Breastfed babies are often healthier and require fewer trips to the doctor with a reduced risk of developing asthma, allergies, diabetes, and obesity.
Benefits for Mom:
- Breastfeeding releases oxytocin, a hormone that helps move milk into the breast.
- It can also help reduce uterine bleeding and assist with returning your uterus to its normal size faster after giving birth.
- Because breastfeeding requires 500 calories a day it might help in some weight loss.
- Breastfeeding saves time and money that would be spent on formula that needs to be mixed and heated up. Breast milk is served naturally, and it's free!
How Do Breast Pumps Work?
How Do Breast Pumps Work?
If you feel as though breast pumps work in mysterious ways and are complex medical devices, don’t worry mama. You’ve got this. They’re actually pretty easy to assemble and use!
- A breast pump emulates a nursing baby by mimicking their natural suckling pattern. As infants nurse, they don't apply constant pressure to the breast. The average baby sucks about 50 to 90 times per minute and slows down once milk is released. An electric breast pump will create this cycle of suction and release by producing one pull per second to initiate milk let down as breast milk begins to flow.
- As breast milk is expressed, it collects in a storage container. The containers are gravity fed so the milk that’s released drips downward into them.
- Breast pumps come with flanges, also known as breast shields, which are funnel-shaped plastic parts that are placed over the nipple and areola to create a seal. The nipple is gently pulled into the flange tunnel to release milk. Make sure you have the correct flange size for pumping success.
"Breast pump suction mirrors baby’s natural sucking through several phases:
Let Down - mimics when baby is vigorously sucking. This phase stimulates the nerves in your breasts, which signals the release of a hormone called oxytocin. The release of oxytocin will make the small muscles that surround your milk-producing tissue contract, which squeezes milk into your ducts.
Expression - mirrors when baby's sucking slows down, and he/she is swallowing milk. This is sometimes called "suck, pause, swallow."
- Leah DeShay, CLEC, IBCLC -
Does Breast Pumping Hurt?
Does Breast Pumping Hurt?
It can but it shouldn't. The first 10 to 15 seconds may be uncomfortable as your nipples begin to stretch and your milk begins to flow, but that generally takes a bit of getting used to. If you experience pain, soreness, or chafing you may need to:
- Change your flange size. If your flange is too big or too small, it can pinch the sides of your nipple and pull the areola inside of the tunnel.
- Change positions. Make sure that your nipple is in the center of your flange. If it's off to one side it can get pulled and pinched in the flange tunnel.
- Adjust the speed and suction settings. If the suction strength or speed is too high, it may cause irritation and discomfort.
- Don't over pump. It takes the breasts about 15 to 30 minutes to empty. Do not pump for more than 30 minutes. If you're having trouble getting your milk to flow, try using a warm compress or massaging your breasts prior to pumping.
"Using a pump should be a similar sensation to comfortable breastfeeding: some pressure and gentle tugging. If you catch yourself dreading the feeling of your pumping sessions or wince while pumping, it is, quite literally, counterproductive to ignore."
- Ashley Georgakopoulos, IBCLC -
Motif Medical Lactation Director
How to Set Up Your New Breast Pump
How to Set Up Your New Breast Pump
Once you receive your breast pump, it may feel overwhelming once you open the box to find tubing, small parts, and bottles. We believe in you, mama! Setting up your pump is easy with just a few simple steps:
- Don’t wait until baby arrives to set up your pump. After your delivery, you don’t want to have to worry about figuring out how to set up your breast pump. Set aside an hour before your due date to put your pump together and to become familiar with how to use it.
- Bust out that instruction manual to learn about how to use your pump. Follow its directions and store it somewhere safe. Your pump manual might have resources for troubleshooting your pump if issues arise. Plus, YouTube is another great resource for learning how to put pump parts together. Some manufacturers have educational videos as well.
- Sterilize your breast pump parts before use. Check to see if your breast pump is dishwasher safe before placing parts in there. Usually, it's recommended to remove breast pump parts from the dishwasher before the drying cycle, as it can warp the parts.
-
Some people may prefer to boil their breast pump parts in water for about five minutes.
-
Medela and Motif make steam clean bags that allow you to sterilize your pump parts in a matter of minutes in the microwave.
-
After your breast pump has been sterilized, allow the parts to completely air dry before storing them or putting the parts together.
If you have a closed system pump, it is not essential to clean the tubing as thoroughly as your other pieces.
It is recommended to thoroughly clean your tubing if you have an open system breast pump.
-
- Take your time. Be patient. Learning can take some time, that’s why it’s important to get started before your little bundle of joy arrives. Most pumps have a variety of suction settings and pumping cycles to become familiar with. While it’s recommended to try on your flanges before your baby is born to make sure they fit, it’s not recommended to try your pump out.
- Plan ahead with breast pump accessories. The breast pump is only the tip of the iceberg! Accessories such as nursing pads, a breast pump tote bag, a hands-free bra, or a nursing pillow could all be added to your registry as essential items to make expressing milk easier and more comfortable.
How to Use a Breast Pump
How to Use a Breast Pump
Now that you know how to set up your breast pump, let’s talk about how to use it. The process is simple, but it can take some practice.
When do I start pumping after baby is born?
After giving birth you can start breast pumping right away (about 1~6 hours afterward) to provide for your infant. If there are no latching issues, you can breastfeed them and wait a few weeks to start pumping.
- Start breast pumping when you’re ready to build and/or store a supply of breast milk. Then remember to stick to your pumping schedule to keep your milk supply consistent.
- If you’re returning to work, try to start pumping a few weeks (if you have that amount of time) before you return. Waiting until the day before might be stressful and frustrating.
- Pump in the morning, that's when moms tend to have the most milk.
- Pump between feedings, either 30 to 60 minutes after nursing or an hour before breastfeeding. This will leave plenty of milk for your baby during the next feeding.
- It’s fine to breastfeed right after pumping, some babies are patient and will feed longer to get the milk they need.
"Sleep is a big topic for new parents. During the first month, you can begin using your breast pump to store milk in order to give your partner the opportunity to feed the baby during the night. This can help your partner have bonding time and share the responsibilities of midnight feeding. It will also give you a chance to practice setting up and using your pump."
Refer to the following instructions to help you breast pump properly:
- Bust out that instruction manual to refresh your memory on how to properly use your pump and to take note of any special features. But generally pumping is as easy as:
- Placing the breast shield on your nipple.
- Turning your electric pump on, or squeezing the mechanism if your pump is manual. - Relax. Find a comfortable place to pump that's free from distractions. Make sure your shoulders are back and your arms are supported. Applying a warm compress to your breasts can enhance let down, the process when your milk begins to flow. Massaging your breasts before and after pumping can also help.
- Stick to a breast pumping schedule. Pumping at the same time each day can help your body produce more milk as demand increases. Also, looking at a picture of your baby or listening to them can help stimulate more milk. Don’t worry if it takes several minutes before your milk begins to flow. Be patient, it’s not immediate at first.
Practicing pumping before you need milk can help your body get used to your pump so you’ll be more comfortable with the process.
How Often Should I Breast Pump?
How Often Should I Breast Pump?
How often you pump depends on a few different factors (such as if you want to build a bigger milk supply, if you’re exclusively breastfeeding, or if you’re going back to work and might be away from your baby regularly).
- If you plan to stay at home with your baby and you're available for breastfeeding, you may only need to pump occasionally. Early on, you should breastfeed or pump 8 to 10 times a day as your milk supply becomes established.
- Your breasts will make more milk when there’s a higher demand for it, so it’s important to breastfeed or pump regularly to boost your supply.
- If your baby feeds regularly and you only want to pump occasionally, it’s best to pump in the morning. It also helps to pump in between feedings, about 30 minutes after or 60 minutes before.
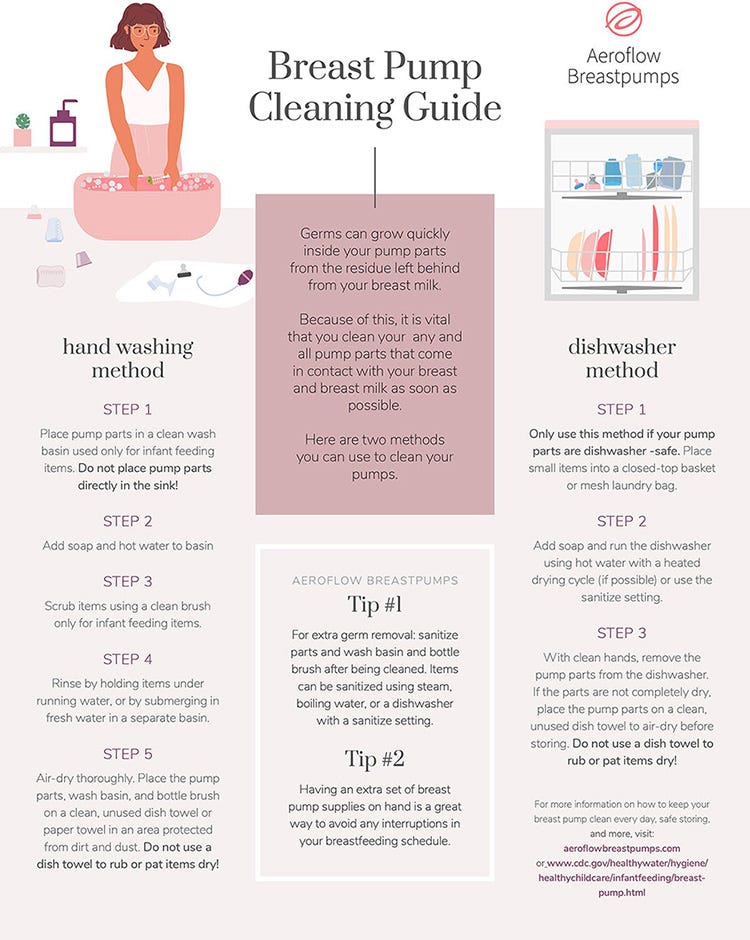
By Hand:
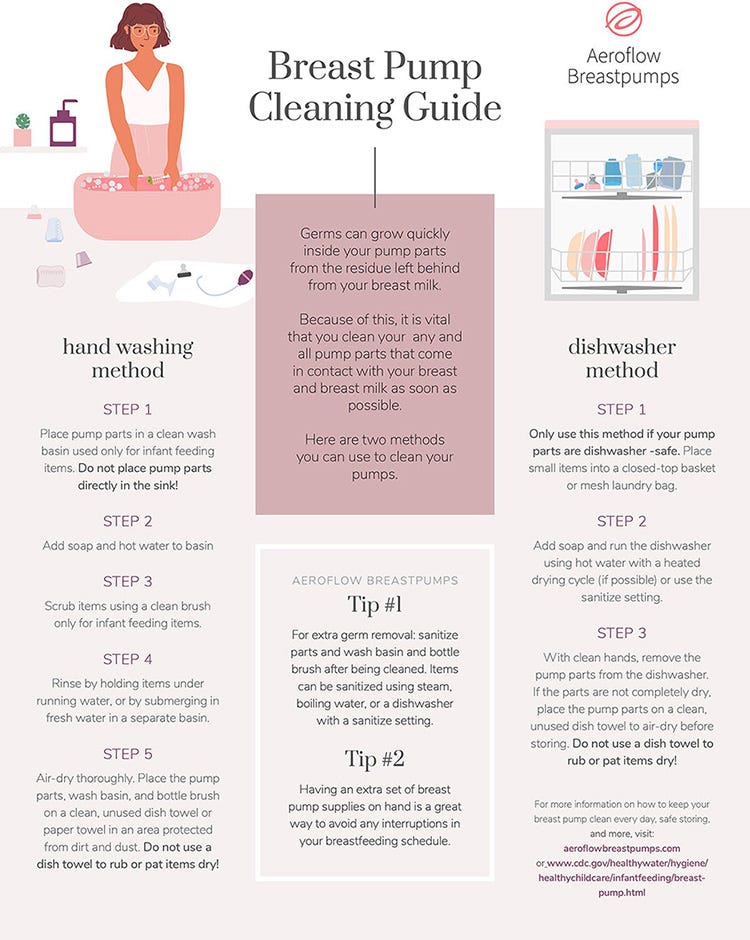
- Use a washbasin. Place pump parts in a clean wash basin used only for washing infant feeding equipment. Do not place parts directly in the sink, because germs in sinks or drains could contaminate the pump.
- Add soap and water. Fill the washbasin with hot water and add soap.
- Scrub. Scrub items according to pump kit manufacturer's guidance. If using a brush, use a clean one that is used only for infant feeding items.
- Rinse. Rinse by holding items under running water, or by submerging in fresh water in a separate basin that is used only for cleaning infant feeding items.
- Dry. Allow to air-dry thoroughly. Place pump parts, washbasin, and bottle brush on a clean, unused dish towel or paper towel in an area protected from dirt and dust. Do not use a dish towel to rub or pat items dry because doing so may transfer germs to the items.
By Dishwasher:
- Wash. Place disassembled pump parts in the dishwasher. Be sure to place small items into a closed-top basket or mesh laundry bag so they don't end up in the dishwasher filter. If possible, run the dishwasher using hot water and a heated drying cycle (or sanitizing setting); this can help kill more germs.
- Remove from the dishwasher. Wash your hands with soap and water before removing and storing cleaned items. If items are not completely dry, place items on a clean, unused dish towel or paper towel to air-dry thoroughly before storing. Do not use a dish towel to rub or pat items dry because doing so may transfer germs to the items.
When Should I Replace My Breast Pump Parts?
There are several indicators that will let you know when it’s time to replace your old parts. The general guideline is that 90 days is the recommended duration between each set of new parts.
- Depending on how frequently you pump, you may have to change your parts before or after the 90-day mark.
- Check your parts for evidence of bacteria buildup or residue.
- This can happen especially in harder-to-reach areas like the tubing.
- You may start to notice your pump not performing as well as it once did. This may be because your valves, which create the strong vacuum suction, are starting to lose elasticity.
- Since not all parts wear out at the same speed, you may only need to stock up on specific pieces.
Some insurances will cover replacement parts periodically for your breast pump, which will save money! Be sure to speak with a Specialist if you are interested in learning more about replacement parts through insurance.
How Much Milk Should I Pump?
How Much Milk Should I Pump?
When breast pumping, be sure to fully empty both breasts. This process could take 25 to 30 minutes. Continue breast pumping for a few minutes after the last few drops of milk have passed to make sure you are done.
The amount of breast milk you produce will vary based on your baby's age, time of day, how often you pump or feed, the quality of your pump, diet, and more.
Based on your child's age, you can expect to pump:
- Days 5 to 7: Up to 2oz.
- Weeks 1 to 3: Up to about 3oz.
- 4 Weeks to 6 Months: Up to 5oz.
Don't worry if you aren't pumping very much breast milk during the first few days after your baby is born. Their stomach is still very tiny, so it's normal to only pump 2 ounces during the first five to seven days.
All moms are different! Some produce more milk and others produce less. If you’re concerned about your breast milk production, speak with your doctor or a lactation professional.
Bonus Breast Pumping Tips!
Bonus Breast Pumping Tips!
Once you get the hang of breast pumping, check out these tips to make your life easier!
- Replace Breast Pump Parts - Your breast pump supplies need to be replaced on a regular basis to keep your pump functioning like brand new and you may qualify for replacement parts through insurance too!
"Worn out breast pump parts are actually the number one cause of decreased milk supply. This is because worn out parts can lead to a decrease in breast pump suction."
- Ashley Georgakopoulos, IBCLC -
Motif Medical Lactation Director
- Let Down and More Milk
If you’re stressed out or pumping at work and can barely get a single drop of milk, try to relax. Save a TV show or book to enjoy only while you pump. Also, photos of your baby or something that smells like them can help produce more milk when you’re away from them. Simulating the warmth of your baby’s mouth with a warm compress, a warm massage, or warm flanges can also increase your breast milk speed and output.
"Using breast massage and hand expression along with pumping with an electric breast pump is the best way to maximize milk output."
- Georganna Cogburn -
MSHE, RD, LDN, IBCLC, RLC
- Storage at Work
When you pump at work, where does your milk go?! You can put it in the fridge, but be sure to label it as yours. Also, separating your milk into smaller portions will help you save milk if your baby doesn’t drink a whole eight ounces.
If you don’t have access to a fridge at work, keep your milk in an insulated cooler with ice or ice packs. Also, using milk storage bags that lay flat is easier for storing because they’re easier to stack.
- Travel and The Airport
Be prepared at the airport, mama. Have your pump ready to pull out of your carry-on bag and place it in a separate bin for the x-ray machine. Tell the agent that you have a breast pump. As a medical item, it will not count as a carry-on. It’s best to have it in your carry-on because you don’t want to be separated from your pump in the event of a delay or if your checked bag is lost.
You can take your breast milk on the plane in quantities higher than 3.4 ounces. Tell the TSA agent that it’s breast milk, and be aware that they may need to test it with a swab.
Getting Your Breast Pump Through Insurance
Getting Your Breast Pump Through Insurance
Aeroflow Breastpumps can help you receive a top-quality, reliable pump through insurance. The Affordable Care Act includes a provision that requires insurance providers to cover breastfeeding support and supplies – including a breast pump.
Our dedicated Specialists will verify your insurance coverage, contact you to discuss your pump options, and even file the insurance claim on your behalf. We work with most major health insurance providers, including Aetna, Blue Cross Blue Shield, Cigna, Tricare, United HealthCare, UMR, Humana, some Medicaid plans, and more.
For detailed information on your insurance coverage, check out these guidelines.
Which Breast Pump is Best?
Ultimately, choosing the best breast pump comes down to your individual needs and personal preferences.