Whether this is your first birth or your tenth, postpartum life can look drastically different from one baby to the next. You may experience a different kind of delivery, new pain, increased or decreased bleeding, or a million other differences.
The good news: this is totally normal! Every birth, just like every new baby, will look and feel different. So, if you want some support while planning for or beginning your postpartum with your new little one, we have compiled our top tips to help make your postpartum experience a happy and healthy one.
IN THIS ARTICLE:
What Are The Primary Postpartum Health Considerations?
How Does Recovery Differ between Vaginal Births and C-Sections?
How Long Does Postpartum Edema Last?
Compression Socks for Pregnancy & Postpartum
When is Postpartum Edema a Problem?
How does postpartum swelling affect breastfeeding?
Postpartum Recovery
What Are The Primary Postpartum Health Considerations?
Most people are aware that there are some risks for both mama and baby during pregnancy, labor, and the postpartum period. But many people come to us with questions about maternal mortality and complication statistics. These concerns are valid—the stats can be scary!—but it’s important to consider these statistics in context.
When considering your risk for developing any pregnancy or postpartum-related complications, first consider your current health status. If you are healthy, there is a lower chance of any complications.
To be clear, these complications are rare. They can happen, but for the vast majority of moms, they simply don’t. In most cases, there is no need to be afraid or concerned. Instead, it’s best to educate yourself so you can recognize any warning signs.
Here are some of the health concerns that could arise during the postpartum period:
- Hemorrhage:
- This is Severe bleeding through the vagina. It may look and feel similar to an extremely heavy period.
- Hemorrhage may occur immediately after delivery or as late as 12 weeks after giving birth.
- Hemorrhage can occur after vaginal delivery or C-section.
- While some bleeding after birth is normal, significant, heavy blood loss is not. If you’re concerned that you’re bleeding too heavily, don’t hesitate to contact your healthcare provider and seek emergency medical attention. Without care, the bleeding may become uncontrolled and life-threatening.
- Infection:
- Because all childbirth involves some trauma to the mother’s body, this naturally increases the risk of contracting an infection. The risk is slightly higher for those who give birth via C-section.
- If you have other risk factors such as obesity, high blood pressure, or diabetes, you have a slightly higher risk of developing infections after birth.
- If small infections are left untreated, they can spread and lead to sepsis, a life-threatening condition in which your body’s immune system turns on itself. Fortunately, most infections are very treatable!
- Heart-Related Problems:
- Potential heart-related complications include postpartum preeclampsia, stroke, blood clots, or heart failure.
- Women who have experienced heart complications with a previous pregnancy may be at a higher risk of developing them again, so it’s important to discuss your previous pregnancies with your current healthcare team.
- Mental Health Issues:
-
- Many new parents experience “the baby blues” — feelings of sadness, anxiety, and overwhelm—in the early days and weeks after giving birth. These feelings should naturally decline within two weeks.
- In some cases, postpartum moms experience more complex postpartum mental health complications. These can include postpartum depression, postpartum anxiety, or postpartum rage. If you think you’re experiencing one of these conditions, don’t suffer in silence. Reach out to your healthcare provider for help.
Warning Signs
What warning signs should you look for? Call your healthcare provider if you experience any of the following:
- A persistent fever above 101 degrees Fahrenheit
- Difficulty breathing
- Chest pain
- Coughing up blood
- Intense headaches
- Thoughts of harming yourself or your baby
- Heavy vaginal bleeding after arriving home
How do you know if your postpartum vaginal bleeding is normal or “heavy”?
A good rule of thumb: If you need to change your pad more than once per hour, that’s a sign to call your doctor.
Postpartum Bleeding
Regardless of how you deliver your baby, you’ll likely experience postpartum vaginal bleeding for up to 6 weeks after delivery. Many people notice bright red bleeding, much like a period, for about a week after giving birth. This period-like bleeding slowly tapers off in the weeks after delivery.
Over the following weeks, the blood will become darker and duller; eventually, it will turn yellow or white. However, many postpartum moms still experience “spurts” of brighter blood—this is completely normal!
IMPORTANT: call your healthcare provider if you experience heavy bleeding or if you need to change your pad more than once per hour at any time during your postpartum period.
Early Recovery
The “early recovery” period occurs during the first 2-6 weeks postpartum. As the name implies, this is the early stage of healing from pregnancy and birth. During these first few weeks, your body needs rest.


Regardless of how you delivered, look out for the following symptoms:
- Increased vaginal bleeding
- Feelings of heaviness in the pelvis
- Increasing pain (it’s normal to have discomfort and soreness around your delivery site, but it should decrease a bit every day)
- Significant changes in the appearance of your incision site (if you had a C-section or stitches used to close vaginal tears). Here are the changes to watch for:
- Increased redness, especially if it’s spreading or streaking in the surrounding skin
- Increased warmth at/around the incision/stitches,
- Foul-smelling or oddly colored discharge from a healing site
- Bleeding from a healing site that had previously stopped bleeding
How Does Recovery Differ between Vaginal Births and C-Sections?
Here is what you can expect based on your delivery method:
- Hospital Stay:
- Vaginal birth in a hospital: Expect to stay in the hospital at least 24-48 hours before you’re discharged. This allows your medical team to monitor you for any signs of postpartum complications.
- C-section: Expect to stay in the hospital for at least 3 nights after your cesarean. Remember, a C-section is a major abdominal surgery, and your medical team needs to monitor you closely for signs of infection or other complications that may arise.
- Vaginal Tears:
- If you delivered vaginally, you may have experienced a vaginal tear or received an episiotomy. Check out this article for more information about healing from vaginal tears and incisions.
- Even if you’ve had a C-section, you may also have a vaginal tear. This can occur if you pushed for a while before the C-section or in cases of twins or triplets (when one child is born vaginally, and another is born via C-section).
- Incision: If you had a c-section, you’ll need to care for your scar. Your doctor will provide specific instructions for scar care. Here are some common recommendations:
- Gently rinse your C-section incision with warm water and gentle soap at least once per day.
- Pat your incision dry with a soft towel.
- Follow any instructions provided by your healthcare provider. Providers have different opinions on whether it’s better to cover the wound or leave it open to air.
- Pain/Lifting: Because a C-section is major abdominal surgery, your abdomen needs time to recover before you return to all your usual activities.
-
- Don’t hesitate to ask your partner, family members, and/or friends for help with general chores and household tasks.
- Avoid lifting anything heavier than your baby for the first few weeks. A pelvic physical therapist or postpartum corrective exercise specialist can help you learn how to bend and lift safely as you recover.
Other Postpartum Healing Tips
Here are a few more tips to help with your recovery and postpartum care:
- Stock up on perineal tear recovery supplies:
- Numbing Spray, Tucks Pads, and a Peri-Bottle. If you’ve experienced a vaginal tear, keep this combo of supplies in your bathroom next to the toilet.
- Each time you pee, you can squirt the peri-bottle across your perineum: this can help decrease stinging sensations during urination.
- After you’re done, pat the surrounding area dry, and if you’d like, apply some numbing spray.
- Place a Tucks pad over your perineum and anus, and if needed, change your pad.
- Numbing Spray, Tucks Pads, and a Peri-Bottle. If you’ve experienced a vaginal tear, keep this combo of supplies in your bathroom next to the toilet.
- Sitz Baths. A sitz bath allows you to cleanse your perineal region without taking a full bath or shower, and it’s an easy way to soothe the healing area. Many mamas purchase a toilet cover made specifically for sitz baths.
- To use a sitz bath, fill the basin up with clean, warm water. Check with your provider before doing sitz baths, but most providers are completely fine with them and encourage their use.
- Combat postpartum constipation.
- Regardless of your delivery method, that first postpartum poop doesn’t feel great. You can improve the experience by ensuring your stool is soft and mobile.
- Ask your healthcare provider if you can use over-the-counter stool softeners to manage constipation.
- Stay hydrated: dehydration makes constipation worse, so stick to a consistent schedule of water intake. Some people find that warm water is particularly helpful for reducing constipation.
- Consider postpartum compression garments.
- A postpartum compression garment can help support your abdomen as it is recovering from delivery.
- These wraps can also reduce pain as you gradually return to daily activities.
- If you’ve had a c-section, a compression garment can provide support to your incision while it heals.
- Your insurance may even cover the cost of the garment; fill out our form to check!
- Take time for yourself. We know this is easier said than done, but make sure you are taking a few minutes a day to focus on yourself. Having a baby is a huge change to your routine. Whether it’s reading, meditating, taking a walk outside, or exercising, make sure you carve out a little time for yourself each day. Enlist friends and family to help you during these short breaks. It’s important to prioritize your mental health as you transition into your new role as a parent!
Postpartum Edema
Postpartum edema, or postpartum swelling, occurs when your tissues retain excess fluid after childbirth. The main symptoms of postpartum edema are weight gain and swollen extremities—most commonly, hands, feet, and ankles.
Postpartum swelling may look similar to pregnancy swelling. It can cause your outer layer of skin to look stretched, shiny, or puffy.
Here are some common factors that can contribute to postpartum edema:
- Hormones: Pregnancy hormones cause your veins to dilate—a necessary adaptation for a healthy pregnancy—and this widening of the veins can cause swelling to develop. After delivery, it takes your body a little while to catch up and process this extra fluid.
- Leftover fluid from pregnancy: While you were pregnant, your body naturally prepared for childbirth by retaining water. This extra fluid helped your body tissues adapt to the baby’s growth. As your baby and uterus grew, they put pressure on a large vein on the right side of your body. This increased pressure compressed the vein and slowed down blood flow through it. When this vein can’t drain quickly enough, excess fluid accumulates in the tissue of the ankles and feet.
- IV fluids administered during childbirth: If you had a c-section, delivered twins, or required medication like Pitocin™ during labor, your healthcare team likely gave you an IV. The extra fluid from the IV can contribute to postpartum swelling.
How Long Does Postpartum Edema Last?
Symptoms usually recede within the first week after childbirth as the kidneys begin to process and eliminate excess fluids. You may notice more swelling on hot summer days or at the end of a long day on your feet.
Everyone’s postpartum body is unique: your body may clear out your swelling quickly, or it might need a bit longer than seven days. If you notice that your swelling is getting significantly worse or has lasted much longer than a week, call your healthcare provider.
You can help your hard-working kidneys by staying hydrated and engaging in gentle, consistent movement like walking. You can also manage edema by wearing special medical garments like compression stockings.
Compression Socks for Pregnancy & Postpartum
Compression socks are a great tool for reducing extremity swelling caused by postpartum edema. Some postpartum people find that compression socks also help reduce discomfort caused by the swelling in their lower legs and ankles.
You might find that you sweat more or urinate a lot in the days after giving birth—this is normal! Your body is working hard to get rid of all the excess fluid. Though it seems counterintuitive, staying well-hydrated will help your body with this process: drink a little more water than you need to quench your thirst. Hydration is particularly important if you’re breastfeeding. Try to drink a glass of water with each meal and each time you feed your baby.


When is Postpartum Edema a Problem?
In most cases, postpartum swelling is nothing to worry about and is merely an inconvenience for new moms. It should only be a concern if it increases significantly and/or you begin experiencing pain.
In the first 6 weeks after delivery, contact your doctor right away if you have persistent swelling in combination with any of the following symptoms:
- A new or sudden increase in swelling
- Severe edema can be dangerous and is associated with a dangerous, life-threatening condition called postpartum preeclampsia.
- Swelling in just one part or on one side of your body
- One leg is warm, red, and painful (this is a sign of possible DVT)
- Severe headache, blurred vision, and sensitivity to light
- Nausea and vomiting
- Chest pain
- Difficulty breathing
- New, rapid weight gain
How does postpartum swelling affect breastfeeding?
Postpartum swelling from IV fluids in labor can lead to excess breast swelling, which may interfere with breastfeeding. If you are experiencing swelling in your breasts and/or your baby is struggling to latch, you can practice reverse pressure softening. Our team of lactation consultants can teach you this technique and help you with other issues that may be hindering your breastfeeding goals.
Can I Take Water Pills?
Any prescription water pill (diuretic) is strongly discouraged during pregnancy. After pregnancy, a diuretic can help alleviate symptoms of swelling, but you should ask your doctor before taking these medications.
Other Tips for Managing Postpartum Swelling
- Sit down and put your legs up. Avoid standing for a long time, and make sure to rest. Don’t cross your legs while sitting, as this reduces circulation. Elevate your legs above your heart for 20-minute periods throughout the day to improve your circulation and reduce swelling. You can pump your ankles up and down in this position to encourage blood flow in the lower legs.
- Get a massage. This is a perfect time to request a massage from your partner! If you aren’t experiencing much pain, have your partner massage your legs and feet gently. This can help promote circulation and reduce swelling.
- Acupuncture treatment. Research indicates that acupuncture can reduce inflammation and improve circulation, so some postpartum people may find that it helps them manage their swelling.
- Stay cool. Keep your body temperature at a steady level and avoid extremely hot environments like saunas. Heat can make swelling worse!
Episiotomy
An episiotomy is an incision in the perineum to make extra room for a baby’s head during childbirth. The perineum is the area between the vagina and anus.
Medical experts no longer recommend routine episiotomies, but in some instances, they may be necessary for a safe delivery. If you experience a scenario that calls for an episiotomy, you should be given a choice and an opportunity for informed consent.
Episiotomy Healing & Self-Care
Healing after an episiotomy can take several weeks. The sutures (stitches) used to close the incision usually dissolve within 6-8 weeks, so they do not need to be removed. To promote optimal healing, keep the area around your incision and stitches as clean and dry as possible. Avoid tampons, sexual intercourse, douching*, and any other activities that might cause the sutures to break for at least six weeks after giving birth.
*Vaginal douching is dangerous and unnecessary for nearly everyone with a vagina. You should never douche unless specifically instructed to do so by your physician.
Cleaning and Care
- Cleaning:
- Keep the healing area clean and dry by changing pads often (every 2 to 4 hours).
- Rinse the perineal area with warm water using a “peri-bottle” each time you urinate or have a bowel movement. Gently pat your incision dry with a clean towel when finished.
- Avoid using soaps in this area, especially those with perfume additives, which can be irritating to the healing tissue.
- You may eat a normal diet after having an episiotomy. A healthy diet high in fiber can help reduce the chance of constipation and the need to strain while using the bathroom. Less straining = less stress on your healing incision! If you’re struggling to maintain soft stool that is easy to pass, ask your healthcare provider if you can use over-the-counter stool softeners to help.
- You may resume physical activity as tolerated. Walking is an excellent way for postpartum moms to be active without overdoing it after episiotomy.
Pain Management
Pain at the incision site is the most common problem moms experience after having an episiotomy. Here are at-home treatments you can use to reduce incision pain.
- Apply ice packs, particularly in the first 24 hours after birth.
- Apply cold packs for 15-20 minutes, 3 to 4 times per day. Give your skin time to recover and warm up between applications.
- After 24 hours, you can alternate between warm and cool compresses.
- Easy hack to make your own perineal ice pack: dunk a clean menstrual pad in water, then place it in the freezer.
- Use a sitz bath of warm water.
- Pain meds: Ask your doctor if you can use an over-the-counter pain reliever such as ibuprofen. You may also be able to use topical numbing sprays, such as benzocaine.
- Consider a cushion. Sitting on a donut-shaped cushion or placing rolled towels underneath your thighs helps to take pressure off areas with stitches or swelling. Resting on either side also takes direct pressure off the perineum.
Episiotomy Symptoms
Worrisome symptoms while healing from an episiotomy include fever or chills, severe perineal pain, bleeding from the incision site, and/or foul-smelling vaginal discharge. These can be signs of an infection, so call your healthcare right away if you notice any of these symptoms.
It’s very important to go to all scheduled visits with your obstetrician or midwife. Don’t hesitate to call your doctor before your follow-up visit if you have any questions or concerns.
Common Questions
When can I have sex again? Most doctors recommend waiting at least six weeks before attempting penetrative sex. This gives the incision site time to heal. Our best tip: listen to your body. If at six weeks you still aren’t feeling ready, it is perfectly okay to wait. If your healthcare provider has examined your incision and feels it has healed well, but you are still experiencing pain with sex, you can ask your provider for a referral to pelvic physical therapy. A pelvic PT can teach you strategies to reduce sensitivity and improve scar mobility—remember, sex should not hurt!
Will I need an episiotomy for future deliveries? Not necessarily! Just because you had an episiotomy with one delivery does not mean you will automatically need one for your next.
Will I tear again? Your initial episiotomy site should be completely healed by the time you are pregnant and laboring with another child, so the incision site will not “tear open.”
What are my options? Before your due date, talk with your OB-GYN or midwife and ask what criteria they use to decide when an episiotomy is necessary. Most practitioners will only suggest an episiotomy if it’s necessary to help advance labor and ensure both mom and baby are safe. You have a right to make your preferences known ahead of time.
Compression Garments
Earlier, we discussed how compression garments can be extremely helpful during pregnancy and postpartum. Here are some garments we recommend:
Maternity Support Band
As your belly grows, your back has to carry a heavier load. A belly band can help support the weight of your bump and make you more comfortable!
Compression Socks
If you’re dealing with postpartum swelling, compression socks can be a game-changer. They can reduce swelling and discomfort and promote blood circulation.
Postpartum Compression Garment
These compression garments are specifically designed to reduce swelling, pain, and discomfort in postpartum bodies. They also provide light, comforting compression to your abdomen, hips, and pelvis – all the areas that are recovering from the strain of childbirth!
Pelvic Health and Bladder Function
Most of us don’t think about our pelvic health very often. We let our pelvic floors work as they’re designed, automatically managing our bladder, bowel, and sexual functions. However, carrying and birthing a baby creates new challenges for the pelvic floor, and often, this can lead to dysfunction. Pregnancy and the postpartum recovery period are opportunities to check in with our overall pelvic health and set it up to function well through the next phases of our lives.
When you consider all the things our pelvis does for us, it’s worth the time and effort to get everything in order after major events like pregnancy and birth!


Why is pelvic health important?
The term “pelvic health” encompasses your gastrointestinal, urinary, reproductive, and sexual health. If your pelvic health isn’t what it should be, you may experience problems with any or all of these systems; poor pelvic health can also cause pain and interfere with daily activities and athletic performance. The physical challenges of pregnancy and postpartum recovery can tax all the structures in and around your pelvis, leading to pelvic health problems.
Here’s the good news: Practically all pelvic health problems that arise during or after pregnancy are very treatable!
Basic Pelvic Anatomy
The pelvic girdle is composed of several bones joined by seven joints. This bony structure shifts around during pregnancy and birth to allow for the baby’s growth and delivery, and it can take up to 12 months to return to its pre-pregnancy position.
The pelvic floor consists of all the structures lining the bottom of the pelvic girdle, including the pelvic floor muscles and their nerves, tendons and ligaments, and connective tissue. The pelvic floor supports the internal pelvic organs, including the bladder, the lower intestines and rectum, and the reproductive organs. The recovery of your pelvic girdle and pelvic floor muscles is a critical part of your postpartum recovery. When they are functioning well, they support your organs and allow you to move and function without pain.
How can I improve my postpartum pelvic health?
Pelvic floor physical therapy is often the first line of treatment for many pelvic floor concerns. Pelvic physical therapists can work with you to help you regain normal pelvic floor function after delivery.
Pelvic floor muscle exercises, or Kegels, can be a helpful strategy for your pelvic floor, but they aren’t a blanket fix for everything! Though they are often broadcast as something “everyone needs to do," people with tense, tight pelvic floor muscles often find that Kegels worsen their issues.
Additionally, up to 50% of women don’t perform kegel exercises correctly, even when they think they understand them! This makes an excellent case for attending pelvic floor physical therapy after every birth, even if it’s just for a visit or two. This is an opportunity for a professional to evaluate your pelvic floor and design a treatment plan specifically for your needs.
Home biofeedback units are increasingly popular tools to help people perform pelvic floor exercises at home. They can be very helpful for new parents who aren’t able to attend in-person pelvic PT frequently. You can insert these Bluetooth-enabled devices into the vagina like a tampon. Once in place, they will measure your pelvic floor muscle activity. Those signals then transmit to your cell phone and allow you to see your pelvic floor contract and relax on the screen.
These devices help you learn to perform pelvic floor exercises correctly, and they allow you to track your progress. However, you should wait to use an internal device until your healthcare provider has assessed your vaginal healing and told you it is safe to use tampons or engage in penetrative sex. Before investing in a biofeedback unit, we highly recommend consulting with a pelvic physical therapist to be sure it’s the right tool for you.
Pelvic Floor Exercises
In addition to kegels, you can exercise your pelvic floor and the neighboring muscles in other ways. For maximum efficacy, perform three sets of 10-15 reps of the following exercises daily:
Bridge

Sit to Stand
Mini Lunges
Rehabbing your abdominal muscles after childbirth will also boost your pelvic health! The deep abdominal wall has a reflexive relationship with the pelvic floor. These muscle groups work as a team to support each other.
With each of the following exercises, engage the pelvic floor and draw the navel up and in to engage the deepest layers of the abdominal wall. Try to avoid flaring your ribs or flattening your lower back. If you see your belly pushing out or you notice you’re holding your breath from effort, you’re probably working too hard! Slow, steady effort is the key to bringing these abdominal muscles back online.
Bent Knee Fall-Out

Low Abdominal Marches

Quadruped Lifts
Modified Side-Plank
Postpartum Pelvic Health Problems
Stress, Urge, and Mixed Urinary Incontinence
Stress urinary incontinence, is a type of bladder leakage that occurs when your bladder and pelvic floor are under physical stress from activity. Leaks when coughing, sneezing, laughing, jumping, or lifting heavy items are among the most common postpartum concerns. Approximately one-third of postpartum women report some degree of incontinence.
While stress incontinence is common after childbirth, it’s not something you have to live with forever! Many new moms find that this leakage improves slightly over the first few weeks of recovery, but most need a little additional help to completely eradicate it (see the section on pelvic floor exercises above for recommendations!)
Other postpartum urinary complaints might include urinary urgency or urge incontinence (feeling the need to suddenly rush to the bathroom but being unable to make it in time) and urinary frequency (peeing more than 4 to 7 times per day). It is also common for postpartum people to experience a mix of these incontinence issues.
Bowel Function
Constipated? Sluggish bowels postpartum can be caused by a combination of factors. Common culprits include:
- Medications you were given during labor
- Postpartum pain management medications
- Dehydration, which may be exacerbated by breastfeeding
- Being less active during recovery
- Dietary changes.
Constipation can lead to a worsening of your pelvic function if you don’t address it, but fortunately, simple adjustments can help reduce constipation.
To combat constipation, focus on whole foods with plenty of fiber and drink 8-10 glasses of water per day.
When you’re sitting on the toilet, try placing a stool under your feet. Elevating your feet optimizes the angle of your colon, making it easier to pass a bowel movement. Don’t hesitate to check in with your healthcare provider or pelvic physical therapist about persistent constipation to learn more strategies to manage constipation.
Sexual Function
Sexual health is a lifelong consideration involving factors that change naturally over time. After you’ve had a baby, sex may not feel appealing for a while. Hormones, healing, mental health, and overall fatigue in the postpartum period can combine to reduce your interest in sex.
Start by discussing these feelings with your partner so they are aware of what you’re experiencing. For the first few months postpartum, prioritize other forms of intimacy like cuddling, kissing, and quality time together.
Many postpartum people find that their sex drive gradually returns in the months after delivery, but some people find they need additional help as they return to sexual activity. Don’t hesitate to discuss further options for sexual healthcare with your healthcare provider, mental health therapist, or pelvic physical therapist.
Pain
You might experience pelvic pain after birth that impacts intercourse, pelvic exams, and activities like carrying your baby, walking, and exercising. No matter the cause, pain is never something to ignore.
Speak to your healthcare provider about your pain or set up a checkup, and don’t settle for dismissive responses. Pelvic physical therapy is an excellent resource for people experiencing pelvic pain and other forms of pain after childbirth.
Mental Health and the Pelvic Floor
Pelvic floor disorders can affect your mental health, and emotions like anxiety, fear, or stress can exacerbate pelvic symptoms, leading to a vicious cycle of problems. These difficult emotions can lead to physical responses like increased tension in the muscles of the pelvic floor. Over time, chronic pelvic muscle tension can lead to issues like pain, urgency, and back pain. It’s worth considering how emotional health might be contributing to your pelvic floor concerns and sharing these potential links with your care provider. There may be more you can do to improve your symptoms.
Postpartum Exercise
Regardless of how you delivered your baby, you can start some simple exercises to help your body regain optimal movement patterns. After all, caring for a newborn requires a lot of movement, even if you have an excellent support system. You’ll be getting up and down out of chairs and couches, rolling over and sitting up in bed, and picking your baby up out of their crib or bassinet at all hours of the day and night.
Though it’s best to keep movement intensity low in the early weeks of the postpartum period, it’s never too early to be mindful of the quality of our movements and establish a foundation that will serve us well later on.
In the early weeks postpartum, focus on reconnecting with your body. There will be plenty of time later on to think about strength! Start slowly and focus on the muscles you’re trying to use.
Here are some exercises to get you started:
- Squats: A squat is a natural progression from the sit-to-stand movement we covered in the pelvic floor exercises above. Continue with the same movement, but take away the chair. Inhale as you squat down, and exhale as you push through your heels to stand.
- Side Plank: When performed correctly, side planks are an excellent way to safely challenge postpartum core muscles. Start by lying on your side, propped up on your elbow. Bend the bottom knee to modify the exercise so that you lift onto your knee instead of your foot. Take a deep breath, and exhale as you draw your core in and lift onto your knee and elbow.
- Lunge: This exercise coordinates the core, pelvic floor, and hip muscles. Start with feet together, standing tall. Step one leg behind you and bend both knees into a lunge, keeping most of your body weight over the front foot. Exhale, draw in your pelvic floor and press through your front foot to return to standing. Repeat on the other side.
- Row: Start with your arms extended, holding the ends of an elastic exercise band. Squeeze the muscles between your shoulder blades to draw your arms back toward you in a rowing motion. Relax your neck and jaw, and focus on letting your back muscles do the work. Visualize pulling your shoulder blades together.
- Low-Impact Cardio: Emphasize long walks, stationary bicycle rides, and elliptical machine workouts during these early weeks. These types of exercises are gentle on the pelvic floor, and they are a great way to work up to more intense, high-impact exercises like running.
Avoid holding your breath during any exercises: breath-holding puts extra strain on the healing abdomen and pelvic floor. If you’re struggling to breathe comfortably during an exercise, it’s likely too advanced: try an easier version of the exercise to see if you’re more successful, then work your way back up to the harder version as you gain strength.
Pregnancy and Postpartum Must-Haves
As you're planning (and likely shopping) for your pregnancy and postpartum needs, let us help you find the products that you need most!
Motif Microwave Steam Sterilizer Bags
No mom wants to use her free time to clean her breast pump. Make cleaning your pumping equipment quick and easy with these sterilizer bags! Just put your accessories inside, put the bag in the microwave for three minutes, and you’re all set to go!
Mama Strut Peri Bottle
We’ve said it once, we’ll say it again: using a peri bottle after birth will save you. It keeps you clean after using the bathroom—no wiping required! It also provides instant relief from stinging or pain when you pee. You can even add sitz bath salts to increase the soothing effect!
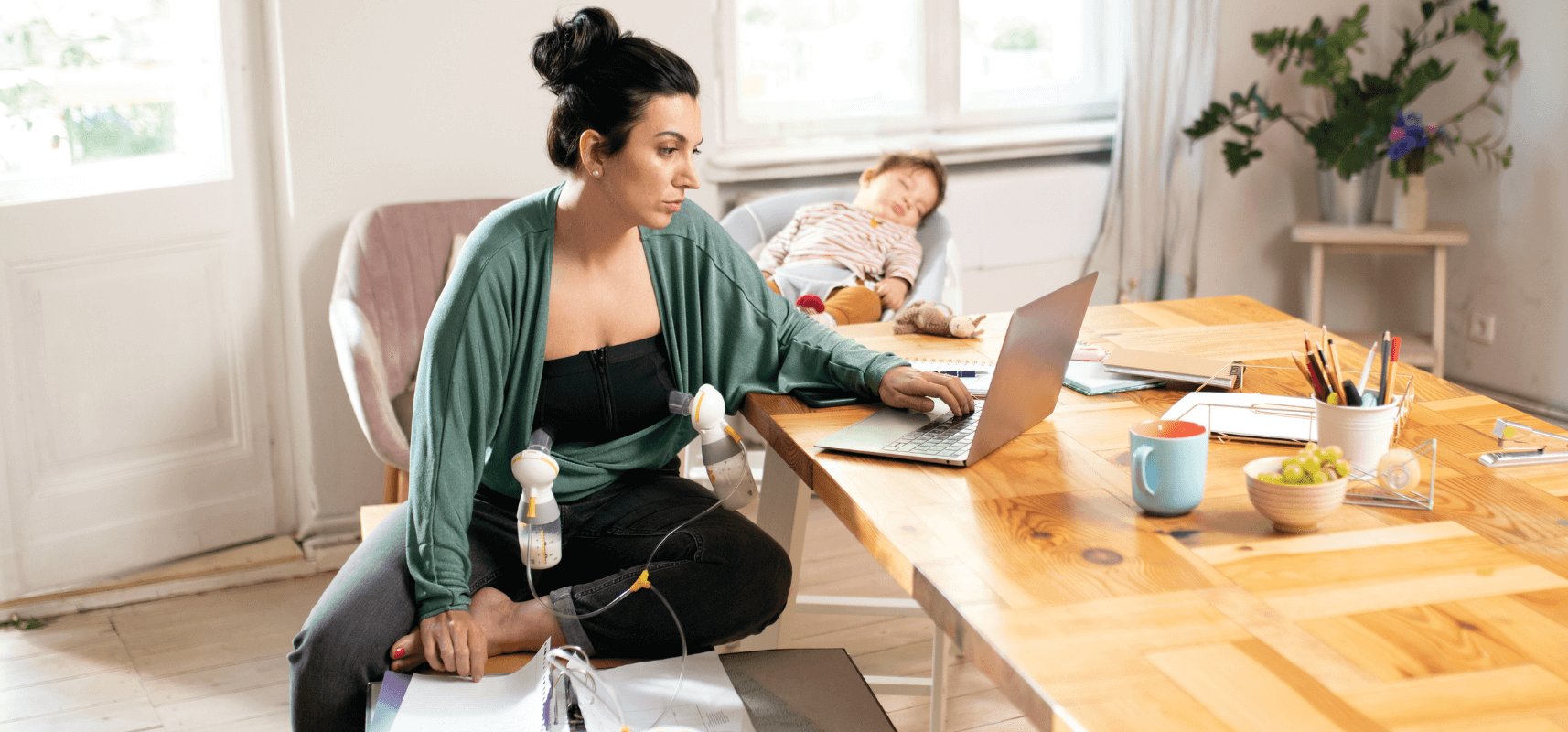
Nursing Bras and Tanks
Regular bras that are too tight can cause sore nipples, clogged ducts, and even breast infection (mastitis). Nursing bras and tanks are worth the convenience and comfort they provide. They are extra stretchy, so you can even wear them during pregnancy to accommodate your ever-changing breasts. After your baby is born, they allow quick and easy access to your breasts for feeding or pumping. Some are even designed to hold your breast pump’s flanges in place so you can pump hands-free!
Breast Pump Bag
These bags are popular and convenient because they keep all your breastfeeding and pumping essentials in one place. You may be able to get a breast pump bag as an insurance upgrade option, but if not, there are several different bags to choose from.
Coolers
Breast milk coolers give moms-on-the-go a safe and convenient way to store and transport breast milk to daycare, from work, or any time you’re out and about. Some even come with extra milk storage containers that work with your breast pump.
Power Options
Nothing is worse than your pump dying when you need it most. If you have an electric breast pump that doesn’t have a battery option, you can still take it on the go in the car with these power options!
Manual Breast Pump
Even if you already have an electric pump that you use daily, you should consider getting a manual breast pump too. They are quick and easy to set up and they don’t require a power source (great backup in case of a power outage or problems with your electric pump). Keep a manual pump in your purse for those moments when errands take longer than expected and you need a quick pumping session to relieve fullness and discomfort!
Nursing Pads
Breastmilk leaks begone! Keep these nursing pads in your bra or nursing tank to prevent leaks from showing through your shirt. You can choose between disposable and washable nursing pads.
References
https://my.clevelandclinic.org/health/diseases/22228-postpartum-hemorrhage
https://www.mayoclinic.org/diseases-conditions/sepsis/symptoms-causes/syc-20351214
https://www.mayoclinic.org/diseases-conditions/postpartum-preeclampsia/symptoms-causes/syc-20376646
https://my.clevelandclinic.org/health/body/17675-blood-clots
https://www.mayoclinic.org/diseases-conditions/postpartum-depression/symptoms-causes/syc-20376617
https://my.clevelandclinic.org/health/diseases/22693-postpartum-anxiety
https://my.clevelandclinic.org/health/diseases/24768-postpartum-rage
https://my.clevelandclinic.org/health/treatments/24137-sitz-bath
https://www.who.int/news-room/fact-sheets/detail/hypertension
https://www.cdc.gov/ncbddd/dvt/infographics/blood-clot-pregnancy-info.html
https://www.mayoclinic.org/diseases-conditions/preeclampsia/symptoms-causes/syc-20355745
https://internationalbreastfeedingjournal.biomedcentral.com/articles/10.1186/s13006-015-0043-8
https://pubmed.ncbi.nlm.nih.gov/15117523/
https://www.mayoclinic.org/healthy-lifestyle/weight-loss/expert-answers/water-retention/faq-20058063
https://my.clevelandclinic.org/health/articles/14611-kegel-exercises
https://my.clevelandclinic.org/health/diseases/22161-urge-incontinence
https://www.ucsfhealth.org/conditions/mixed-incontinence-in-women